Hyperemesis gravidarum
Hyperemesis gravidarum-
Hyper- Excessive
Emesis- Vomit
Gravidarum-Pregnancy
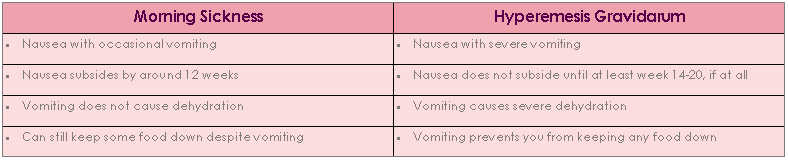
Hyperemesis gravidarum refers to excessive nausea and vomiting that results in fluid and electrolyte imbalance, nutritional deficits, marked weight loss occurring in up to 1 percent of pregnant women and begins before the 20th weeks of pregnancy. Earlier it used to be a contributing factor for maternal mortality.
Etiology
- It remains obscure. However certain facts and theories are known:
- Unknown
- Nulliparity
- Smoking
- It occurs frequently among young obese primigravidas in multifoetal gestation and in trophoblastic diseases. It tends to recur in subsequent pregnancies.
- Theories-
- Hormonal- Excess of chorionic gonadrophin and progesterone.
- Psychogenic
- Deficiency of Vitamin B and disturbance of carbohydrate metabolism.
- Allergic
Clinical Manifestations
- Evidences of starvation and malnutrition.
- Nausea and vomiting are increased.
- Oral feeds are intolerable.
- Oliguria
- Epigastric pain
- Constipation
- Fatigue
- Dry coated tongue
- Sunken eyes
- Ketosis
- Progressive emaciation with dehydration and weight loss.
- Mild pyrexia, tachycardia, breath becomes acetone smell and systolic blood pressure falls below 100 mm of Hg.
Investigations
- History
- Clinical Features
- Urine analysis for volume, colour, specific gravity, pigments and appearance of acetone.
- Estimates of blood value — Haematocrit, Electrolyte levels.
- Thyroid function test
- Ultrasound scan
Nursing Goals
- Reducing and eliminating nausea and vomiting
- Restoring fluid and electrolyte balance
- Coping with the psychological tasks of pregnancy and motherhood
- Continuing foetal growth and development.
Nursing Interventions
- Obtain history for accessing pattern of nausea and vomiting
- A complete physical examination about fluid and electrolyte imbalance, nutritional status and signs of complications such as metabolic acidosis and jaundice.
- Administration of parenteral and enteral fluids and electrolytes and antiemetics.
- Maintain observation chart.
- Encourage patient to sit upright after meal.
- Provide a hygienic, restful and odourless environment.
- Check for elimination especially bowel movement and maintain intake and output chart.
- When there is response to therapy start with limited oral fluids and carbohydrate foods like biscuits, bread and toast.
- Monitor maternal and foetal well-being.
Complications-
- Dehydration-Electrolyte imbalance, renal failure
- Wernicke’s Encephalopathy (Thiamine deficiency)
- Vitamin K deficiency- maternal coagulopathy or fetal intracranial haemorrhage
- Mallory Weiss tears- Characterized by upper gastro-intestinal bleeding secondary to longitudinal mucosal lacerations at the gastroesophageal junction or gastric cardia.
- Boerhaave syndrome- Characterized by upper gastrointestinal bleeding secondary to transmural perforation of the esophagus (Boerhaave syndrome is thought to be the result of a sudden rise in internal esophageal pressure produced during vomiting, as a result of neuromuscular incoordination causing failure of the cricopharyngeus muscle to relax.)