Second Stage of labour
Second Stage of labour-
The basic principles in the management of the woman in the second stage of labour is to prevent injury to the mother and the foetus. The duration of second stage varies. In multigravida it may last as little as 5 minutes. In primigravida, it may take two hours. Average duration is around 1 hour in Primigravida and 30 minutes in Multigravida.
This stage has two phases-
- Latent phase - The latent phase is from the onset of labour until the cervix reaches 3 cm dilatation,
- The active phase is from 3cm dilatation to complete dilatation of the cervix, i.e., 10 cm
Physiological Changes
A knowledge about physiological processes will help the midwife in managing women in second stage of labour. You will now see what are the changes.
- Stronger and More Frequent Contractions
The contractile power of the uterus is intensified because the foetus is closely applied to the uterus, as some of the fluid has escaped. The upper uterine segment becomes short and thick because of the retraction of uterine muscle fibres. During each contraction, its force is transmitted through the long axis of the foetus, directing it through the birth canal. This is known as the foetal axis pressure.
2. Expulsive Action of the Abdominal Muscles and Diaphragm
The abdominal muscles and diaphragm contracts, known as ‘bearing down’ or ‘pushing’. Initially it is reflex, but can be aided by voluntary effort. With the distension of the pelvic floor by the presenting part, the expulsive action becomes involuntary.
3. Displacement of the Pelvic Floor
The bladder is drawn up into the abdomen, the vagina is dilated by the advancing head, the posterior segment of the pelvic floor is pushed downwards in front of the presenting part and the reaction is compressed by the advancing head. Further changes that takes place is pouting and gaping of the anus, thinning out of the perineum and lengthening of the posterior wall of the birth canal.
4. Expulsion of the Foetus
The head is visible at the vulva. With each contraction it advances and recedes till crowing takes place. The head is born by extension, after which the shoulders and body is born, with the remaining amniotic fluid.
Nursing Management of Women in second Stage of Labour-
It is very important for the nursing personnel to recognise the commencement of the second stage. There are many probable signs that indicate the transition from first to second stage. There is only one positive sign.
- Positive Signs
- On vaginal examination
- No cervix is felt
2. Probable signs
- Expulsive uterine contractions- The woman has a strong inclination to bear down.
- Trickling of blood- It is due to mild laceration of the cervix that takes place when it is stretched and laceration of the vaginal mucous when the head descends down.
- Rupture of the membranes may take place.
- Pouting and gaping of the anus- This occurs when the head has reached the pelvic floor. When the anus gapes and faeces are expelled, the cervix is usually dilated.
- Tenseness between anus and coccyx- This can be assessed by applying pressure with the middle finger between the anus and the coccyx. This tenseness is because of the pressure exerted by the descending head on the rectum and pelvic floor.
- Congestion and gaping of the vulva.
- Presenting part appears. This is considered as the probable sign because in some cases like footling breech presentation, the foot may appear, although the cervix is not dilated completely or if excessive moulding of head is present.
- A caput may appear.
Observation- Maternal and Foetal Condition
The factors that determine the safety of the second stage and must be carefully observed are-
Uterine Contractions
The strength, length and frequency of contractions should be assessed continuously. In comparison to the first stage, it is stronger, the duration is longer (1 minute), with a longer resting phase.
The Descent
The progress is observed by noting the descent. It accelerates during the active phase. If there is delay, a vaginal examination should be performed to note whether internal rotation of the head has taken place to note the station of the presenting part and for presence of caput succedaneum.
Foetal Condition
- Observation of colour of liquor amnii (for meconium staining)
- Changes in foetal heart pattern
Maternal Condition
- Physical ability
- Coping ability
- Pulse rate every 15 minutes
- Blood pressure half hourly
General Care of Woman
Women in the second stage of labour will feel exhausted, and may not have the ability to care for self. You as a nurse will have to give best possible care to the woman and help her to cope with this stage of labour. The care includes-
- Maternal comfort and hygiene
- Sponge the face and neck of the mother with a wet towel.
- Provide ice-chips or sips of water
- Apply moisturizing cream to lips to prevent dryness and cracking
Bladder Care
Encourage to pass urine at the beginning of the second stage if she hasn’t done it during the late first stage.
Pain Relief
Apply measures like massaging, encourage deep breathing, distraction, etc., to relieve pain.
Psychological Care
Reassure the woman. Encourage her to bear down only when instructed to.
Maternal Position
There are several factors that will affect the decision for adopting a specific position, i.e., the maternal and foetal condition, the need for frequent monitoring, the woman’s personal choice, the environment; is it safe? Is privacy provided? and the midwives’ confidence in her skills to assist in the delivery process. Some of the positions that can be adopted are-
Semi-recumbent or supported sitting
This increases the efficiency of the uterine contractions and prevents hypotension and reduced placental perfusion.
Squatting, kneeling or standing
The squatting position increases the transverse diameter by 1 cm and the anteroposterior diameter by 2 cm, thereby resulting in easy delivery. The kneeling and standing position also contributes to easy delivery.
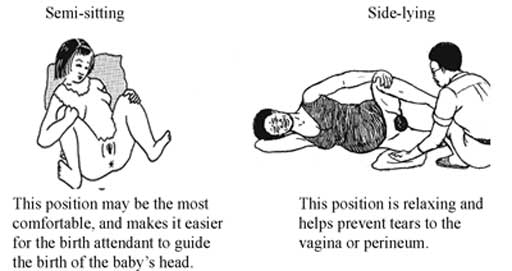
Left lateral position
The midwife can view the perineum clearly. This position is useful for women who cannot abduct their hips.
Bearing Down Effort
The woman should be helped to avoid ‘active pushing’ before the vertex is visible at the vulva. This will allow the mother to conserve her effort and will permit the vaginal tissues to stretch passively. Once the head becomes visible, the mother should be encouraged to follow her own inclinations in relation to expulsive efforts.
Conducting the Delivery
To avoid complications in the mother as well as the new-born, one must conduct the delivery very skilfully. You will now learn about the conduct of delivery in a vertex presentation.
The two phases of delivery of the foetus in a vertex presentation are-
- Delivery of the head, and
- Delivery of the shoulders and body.
The principles to be kept in mind while conducting the delivery is to minimise maternal and foetal trauma and ensure a safe delivery for the baby. Principle of asepsis must be maintained.
Delivery of the head
The perineum is swabbed and the woman is draped with sterile towels. A pad is used to cover the anus. With each contraction the head descends and the superficial muscles of the pelvic floor especially the transverse perineal muscles are visible. During the resting phase, the head recedes, thereby the muscle thins gradually. The midwife places her fingers on the advancing head to monitor descent and prevent expulsive crowning. Once crowned, and episiotomy is given, the head is born by extension. The baby’s neck is checked for cord around it. If it is loose, it is passed through the head, if tight, it is cut.

Delivery of the shoulders and the body
When external rotation of the head occurs, it shows that the shoulders are rotating internally into the antero posterior diameter of the pelvic outlet. While waiting for this to occur, mucus from the baby’s mouth and nostrils may be wiped with a gauze swab. Placing the hand on each side of the baby’s head, over the ears, and applying downward traction, the anterior shoulder is born. The anterior shoulder slips below the symphysis pubis. The head is then guided in an upward direction towards the mother’s abdomen so that the posterior shoulder can escape over the perineum. As soon as the baby is born, the cord is cut, eyes are cleaned, airway is cleared and the Apgar score is noted.
