Pituitary gland
The endocrine system consists of a number of distinct glands and some tissues in other organs. Although the hypothalamus is classified as a part of the brain and not as an endocrine gland it controls the pituitary gland and has an indirect effect on many others. The endocrine glands are:
- 1 Pituitary gland
- 1 Thyroid gland
- 4 Parathyroid glands
- 2 Adrenal (suprarenal) glands
- The pancreatic islets (islets of Langerhans)
- 1 Pineal gland or body
- 1 Thymus gland
- 2 Ovaries in the female
- 2 Testes in the male
Pituitary gland-
Pituitary gland or hypophysis is a small endocrine gland with a diameter of 1 cm and weight of 0.5 to 1 g. It is situated in a depression called ‘sella turcica’, present in the sphenoid bone at the base of skull. It is connected with the hypothalamus by the pituitary stalk or hypophyseal stalk.
Blood supply
Arterial blood
This is supplied by branches from the internal carotid artery. The anterior lobe is supplied indirectly by blood that has already passed through a capillary bed in the hypothalamus but the posterior lobe is supplied directly.
Venous blood
This comes from both lobes, containing hormones, and leaves the gland in short veins that enter the venous sinuses between the layers of dura mater.
Division of Pituitary Gland-
Pituitary gland is divided into two divisions-
- Anterior pituitary or adenohypophysis
- Posterior pituitary or neurohypophysis.
- Anterior pituitary or adenohypophysis-
Anterior pituitary is also known as the master gland because it regulates many other endocrine glands through its hormones.
Parts-
Anterior pituitary consists of three parts -
- Pars distalis
- Pars tuberalis
- Pars intermedia.
Anterior pituitary has two types of cells, which have different staining properties
- Chromophobe cells
- Chromophil cells.
Chromophobe Cells
Chromophobe cells do not possess granules and stain poorly. These cells form 50% of total cells in anterior pituitary. Chromophobe cells are not secretory in nature, but are the precursors of chromophil cells.
Chromophil Cells
Chromophil cells contain large number of granules and are darkly stained. Types of chromophil cells Chromophil cells are classified by two methods.
A. Classification on the basis of staining property-
Chromophil cells are divided into two types-
- Acidophilic cells or alpha cells, which form 35%
- Basophilic cells or beta cells, which form 15%.
B. Classification on the basis of secretory nature-
Chromophil cells are classified into five types-
- Somatotropes, which secrete growth hormone
- Corticotropes, which secrete adrenocorticotropic hormone
- Thyrotropes, which secrete thyroid-stimulating hormone (TSH)
- Gonadotropes, which secrete follicle-stimulating hormone (FSH) and luteinizing hormone (LH)
- Lactotropes, which secrete prolactin
Releasing and Inhibitory Hormones Secreted by Hypothalamus
- Growth hormone-releasing hormone (GHRH): Stimulates the release of growth hormone
- Growth hormone-releasing polypeptide (GHRP): Stimu lates the release of GHRH and growth hormone
- Growth hormone-inhibitory hormone (GHIH) or somatostatin: Inhibits the growth hormone release
- Thyrotropic-releasing hormone (TRH): Stimulates the release of thyroid stimulating hormone
- Corticotropin-releasing hormone (CRH): Stimulates the release of adrenocorticotropin
- Gonadotropin-releasing hormone (GnRH): Stimulates the release of gonadotropins, FSH and LH
- Prolactin-inhibitory hormone (PIH): Inhibits prolactin secretion. It is believed that PIH is dopamine.
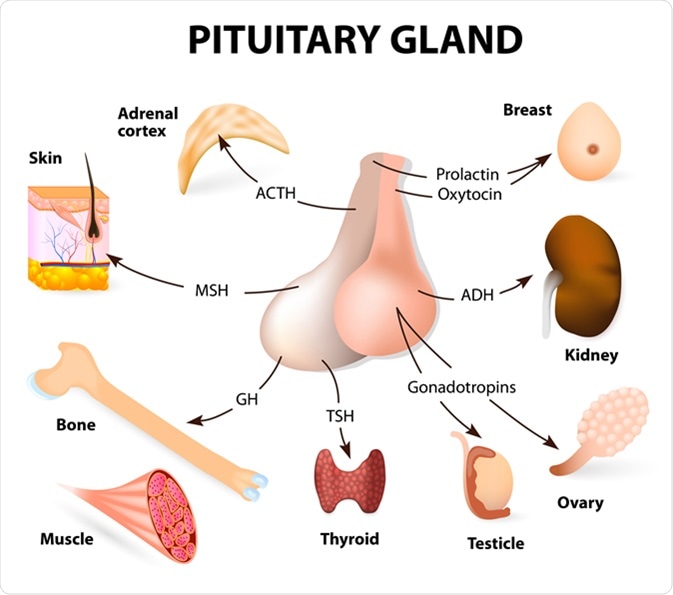
Hormones Secreted by Anterior Pituitary –
Six hormones are secreted by the anterior pituitary-
- Growth hormone (GH) or somatotropic hormone (STH)- is secreted by somatotropes which are the acidophilic cells of anterior pituitary.
- Thyroid-stimulating hormone (TSH) or thyrotropic hormone- This hormone is synthesised by the anterior pituitary and its release is stimulated by TRH from the hypothalamus. It stimulates growth and activity of the thyroid gland, which secretes the hormones thyroxine (T4) and triiodothyronine (T3). Release is lowest in the early evening and highest during the night.
- Adrenocorticotropic hormone (ACTH)- Corticotrophin releasing hormone (CRH) from the hypothalamus promotes the synthesis and release of ACTH by the anterior pituitary. This increases the concentration of cholesterol and steroids within the adrenal context and the output of steroid hormones, especially cortisol. ACTH levels are highest at about 8 a.m. and fall to their lowest about midnight, although high levels sometimes occur at midday and 6 p.m
- Follicle-stimulating hormone (FSH)- Follicle-stimulating hormone is a glycoprotein made up of one α-subunit and a β-subunit. The α-subunit has 92 amino acids and β-subunit has 118 amino acids. The half-life of FSH is about 3 to 4 hours.
- Luteinizing hormone (LH) in females or interstitialcell-stimulating hormone (ICSH) in males - LH is a glycoprotein made up of one α-subunit and one β-subunit. The α-subunit has 92 amino acids and β-subunit has 141 amino acids. The half-life of LH is about 60 minutes.
- Prolactin- This hormone stimulates lactation (milk production) and has a direct effect on the breasts immediately after parturition (childbirth). The blood level of prolactin is stimulated by prolactin releasing hormone (PRH) released from the hypothalamus and it is lowered by prolactin inhibiting hormone (PIH, dopamine) and by an increased blood level of prolactin. After birth, suckling stimulates prolactin secretion and lactation. The resultant high blood level is a factor in reducing the incidence of conception during lactation.
| Hormone | Function |
| Growth hormone (GH) |
Regulates metabolism, promotes tissue growth especially of bones and muscles |
| Thyroid stimulating hormone (TSH) |
Stimulates growth and activity of thyroid gland and secretion of T3 and T4 |
| Adrenocorticotrophic hormone (ACTH) |
Stimulates the adrenal cortex to secrete glucocorticoids |
| Prolactin (PRL) |
Stimulates milk production in the breasts |
| Follicle stimulating hormone (FSH) | Stimulates production of sperm in the testes, stimulates secretion of oestrogen by the ovaries, maturation of ovarian follicles, ovulation |
| Luteinising hormone (LH) | Stimulates secretion of testosterone by the testes, stimulates secretion of progesterone by the corpus luteum |
2. Posterior pituitary or neurohypophysis.
Posterior pituitary consists of three parts-
- Pars nervosa or infundibular process
- Neural stalk or infundibular stem
- Median eminence.
Posterior pituitary is made up of neural type of cells called pituicytes and unmyelinated nerve fibers.
Pituicytes
Pituicytes are the fusiform cells derived from glial cells. These cells have several processes and brown pigment granules. Pituicytes act as supporting cells and do not secrete any hormone.
Unmyelinated Nerve Fibers
Unmyelinated nerve fibers come from supraoptic and paraventricular nuclei of the hypothalamus through the pituitary stalk.
Other Structures
Posterior pituitary also has numerous blood
Hormones of posterior Pituitary-
- Oxytocin- Oxytocin stimulates two target tissues during and after parturition (childbirth): uterine smooth muscle and the muscle cells of the lactating breast. Oxytocin is secreted mainly by paraventricular nucleus of hypothalamus. It is also secreted by supraoptic nucleus in small quantity and it is transported from hypothalamus to posterior pituitary through the nerve fibers of hypothalamo-hypophyseal tract.
- Antidiuretic hormone (ADH) or vasopressin- The main effect of antidiuretic hormone is to reduce urine output (diuresis is the production of a large volume of urine). Antidiuretic hormone (ADH) is secreted mainly by supraoptic nucleus of hypothalamus. It is also secreted by paraventricular nucleus in small quantity. From here, this hormone is transported to posterior pituitary through the nerve fibers of hypothalamo-hypophyseal tract, by means of axonic flow.
Disorders of pituitary gland
| Parts involved | Hyperactivity | Hypoactivity |
| Anterior pituitary |
|
|
| Posterior pituitary | Syndrome of inappropriate hypersecretion of ADH (SIADH) | Diabetes insipidus |
| Anterior and posterior pituitary | ------ | Dystrophia adiposogenitalis |