Thyroid Gland
Thyroid Gland
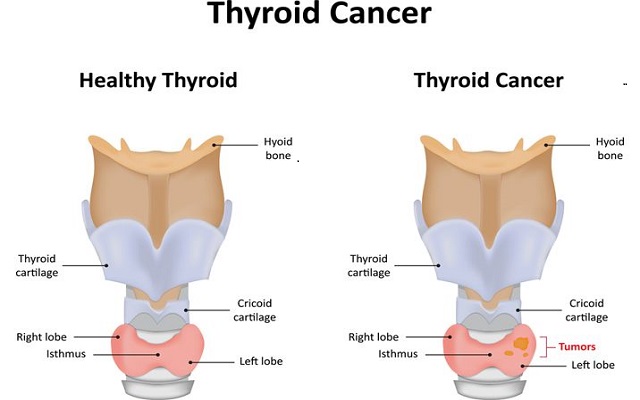
Thyroid is an endocrine gland situated at the root of the neck on either side of the trachea at the level of the 5th, 6th and 7th cervical and 1st thoracic vertebrae. It has two lobes, which are connected in the middle by an isthmus. It weighs about 20 to 40 g in adults. Thyroid is larger in females than in males. The structure and the function of the thyroid gland change in different stages of the sexual cycle in females. Its function increases slightly during pregnancy and lactation and decreases during menopause.
The lobes are roughly cone-shaped, about 5 cm long and 3 cm wide.
The arterial blood supply to the gland is through the superior and inferior thyroid arteries. The superior thyroid artery is a branch of the external carotid artery and the inferior thyroid artery is a branch of the subclavian artery.
The venous return is by the thyroid veins which drain into the internal jugular veins.
Two parathyroid glands lie against the posterior surface of each lobe and are sometimes embedded in thyroid tissue. The recurrent laryngeal nerve passes upwards close to the lobes of the gland and on the right side it lies near the inferior thyroid artery.

Hormones of Thyroid Gland-Thyroid gland secretes three hormones-
- Tetraiodothyronine or T4 (thyroxine)
- Tri-iodothyronine or T3
- Calcitonin.
T4 is otherwise known as thyroxine and it forms about 90% of the total secretion, whereas T3 is only 9% to 10%.
Chemistry- T4 and T3 are iodine-containing derivatives of amino acid tyrosine.
Rate of Secretion-
Thyroxine = 80 to 90 µg/day
Tri-iodothyronine = 4 to 5 µg/day
Reverse T3 = 1 to 2 µg/day.
Plasma Level-
Total T3 = 0.12 µg/dL
Total T4 = 8 µg/dL.
Metabolism of Thyroid Hormones
Degradation of thyroid hormones occurs in muscles, liver and kidney.
Synthesis of Thyroid Hormones-
Synthesis of thyroid hormones takes place in thyroglobulin, present in follicular cavity. Iodine and tyrosine are essential for the formation of thyroid hormones. Iodine is consumed through diet. It is converted into iodide and absorbed from GI tract. Tyrosine is also consumed through diet and is absorbed from the GI tract.
For the synthesis of normal quantities of thyroid hormones, approximately 1 mg of iodine is required per week or about 50 mg per year.
Synthesis of thyroid hormones occurs in five stages-
- Thyroglobulin synthesis
- Iodide trapping
- Oxidation of iodide
- Transport of iodine into follicular cavity
- Iodination of tyrosine
- Coupling reaction
Storage of Thyroid Hormones-
The thyroid hormones remain in the form of vesicles within thyroglobulin and are stored for long period. Each thyroglobulin molecule contains 5 or 6 molecules of thyroxine. There is also an average of 1 tri-iodothyronine molecule for every 10 molecules of thyroxine.
Thyroid gland is unique in this, as it is the only endocrine gland that can store its hormones for a long period of about 4 months. So, when the synthesis of thyroid hormone stops, the signs and symptoms of deficiency do not appear for about 4 months.
Function of Thyroid Hormones-
Thyroid hormones have two major effects on the body-
- To increase basal metabolic rate- Thyroxine increases the metabolic activities in most of the body tissues, except brain, retina, spleen, testes and lungs. It increases BMR by increasing the oxygen consumption of the tissues. The action that increases the BMR is called calorigenic action.
- To stimulate growth in children-Thyroid hormone increases the synthesis of proteins in the cells.
Calcitonin-
Calcitonin This hormone is secreted by the parafollicular or C-cells in the thyroid gland. It acts on bone and the kidneys to reduce the blood calcium (Ca2+) level when it is raised. It reduces the reabsorption of calcium from bones and inhibits reabsorption of calcium by the renal tubules. Its effect is opposite to that of parathyroid hormone (PTH, parathormone), the hormone secreted by the parathyroid glands. Release of calcitonin is stimulated by an increase in the blood calcium level. This hormone is important during childhood when bones undergo considerable changes in size and shape.
Disorders of Thyroid Gland-
Increased secretion of thyroid hormones is called hyperthyroidism.
Hyperthyroidism is caused by-
- Graves’ disease-Graves’ disease is an autoimmune disease and it is the most common cause of hyperthyroidism. In Graves’ disease, the B lymphocytes (plasma cells) produce autoimmune antibodies called thyroid-stimulating autoantibodies (TSAbs).

- Thyroid adenoma- A localized tumor develops in the thyroid tissue. It is known as thyroid adenoma and it secretes large quantities of thyroid hormones. It is not associated with autoimmunity
Signs and Symptoms of Hyperthyroidism
- Intolerance to heat as the body produces lot of heat due to increased basal metabolic rate caused by excess of thyroxine
- Increased sweating due to vasodilatation
- Decreased body weight due to fat mobilization
- Diarrhoea due to increased motility of GI tract
- Muscular weakness because of excess protein catabolism
- Nervousness, extreme fatigue, inability to sleep, mild tremor in the hands and psychoneurotic symptoms such as hyperexcitability, extreme anxiety or worry. All these symptoms are due to the excess stimulation of neurons in the central nervous system
- Toxic goitre
- Tachycardia and atrial fibrillation
- Systolic hypertension
- Cardiac failure
- Oligomenorrhea or amenorrhea
- Exophthalmos
- Polycythemia

Hypothyroidism-
Decreased secretion of thyroid hormones is called hypothyroidism. Hypothyroidism leads to myxoedema in adults and cretinism in children.
Myxedema
Myxedema is the hypothyroidism in adults, characterized by generalized oedematous appearance. Common cause of myxoedema is the autoimmune disease called Hashimoto’s thyroiditis.
Signs and symptoms of myxedema-
- Swelling of the face
- Bagginess under the eyes
- Non-pitting type of edema, i.e. when pressed, it does not make pits and the edema is hard. It is because of accumulation of proteins with hyaluronic acid and chondroitin sulfate, which form a hard tissue with increased accumulation of fluid
- Atherosclerosis- It is the hardening of the walls of arteries because of accumulation of fat deposits and other substances. In myxedema, it occurs because of increased plasma level of cholesterol which leads to deposition of cholesterol on the walls of the arteries.
Cretinism
Cretinism is the hypothyroidism in children, characterized by stunted growth.
Causes for cretinism
Cretinism occurs due to congenital absence of thyroid gland, genetic disorder or lack of iodine in the diet.
Features of cretinism
- A newborn baby with thyroid deficiency may appear normal at the time of birth because thyroxine might have been supplied from mother. But a few weeks after birth, the baby starts developing the signs like sluggish movements and croaking sound while crying. Unless treated immediately, the baby will be mentally retarded permanently.
- Skeletal growth is more affected than the soft tissues. So, there is stunted growth with bloated body. The tongue becomes so big that it hangs down with dripping of saliva. The big tongue obstructs swallowing and breathing. The tongue produces characteristic guttural breathing that may sometimes choke the baby.
Goiter
Goiter means enlargement of the thyroid gland. It occurs both in hypothyroidism and hyperthyroidism.
Goiter in Hyperthyroidism – Toxic Goiter
Toxic goiter is the enlargement of thyroid gland with increased secretion of thyroid hormones, caused by thyroid tumor.

Goiter in Hypothyroidism – Non-toxic Goiter
Non-toxic goiter is the enlargement of thyroid gland without increase in hormone secretion. It is also called hypothyroid goiter Based on the cause, the non-toxic hypothyroid goiter is classified into two types.
- Endemic colloid goiter- Endemic colloid goiter is the non-toxic goiter caused by iodine deficiency. It is also called iodine deficiency goiter. Iodine deficiency occurs when intake is less than 50 µg/day.
- Idiopathic non-toxic goiter- Idiopathic non-toxic goitre is the goiter due to unknown cause. Enlargement of thyroid gland occurs even without iodine deficiency. The exact cause is not known. It is suggested that it may be due to thyroiditis and deficiency of enzymes such as peroxidase, iodinase and deiodinase