Chronic obstructive pulmonary diseases
Chronic obstructive pulmonary diseases
- Chronic Obstructive pulmonary disease is a group of progressive lung diseases.
- COPD is also known as chronic obstructive lung disease (COLD), chronic obstructive airway disease (COAD), chronic airflow limitation (CAL) and chronic obstructive respiratory disease (CORD)
- Chronic obstructive pulmonary disease (COPD) refers to chronic bronchitis and Emphysema, a pair of two commonly coexisting diseases of the lungs in which the airways become narrowed.
- if untreated, COPD can lead to a faster progression of disease, heart problems, and worsening respiratory infections.
This leads to a limitation of the flow of air to and from the lungs causing shortness of breath.
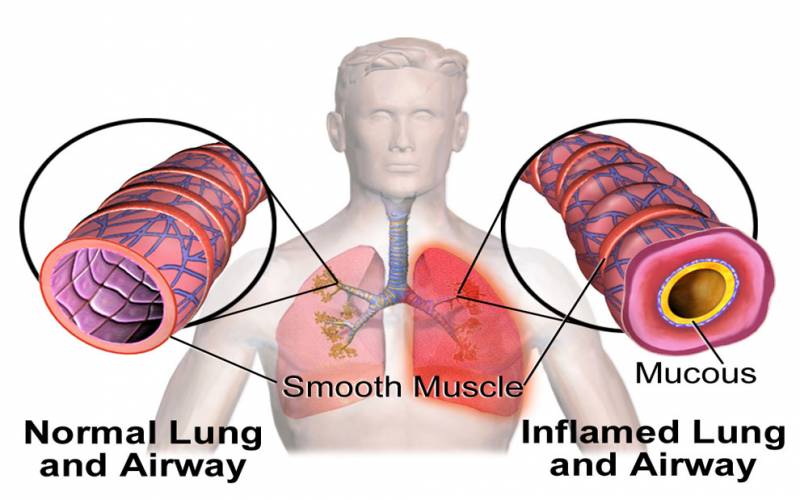
In COPD, less air flows in and out of the airways because of one or more of the following
- The airways and air sacs lose their elastic quality.
- The walls between many of the air sacs are destroyed.
- The walls of the airways become thick and inflamed.
- The airways make more mucus than usual, which tends to clog them.
Incidence
- It is the 4th leading cause of mortality and 12th leading cause of disability in the united states.
- In 2020 COPD is the 3rd leading cause of death.
CAUSES
Smoking- Smoking is primary risk factors for COPD. The numerous irritants found in cigarette smoke stimulate excess mucus production and coughing, destroy ciliary function and lead to inflammation and damage of bronchiolar and alveolar walls.
Air pollution
Air pollution high levels of urban air pollution are harmful to persons with existing lung disease. However, the effect of outdoor air pollution as a risk factor for COPD. Another risk factor for COPD development is fossil fuels that used for indoor heating and cooking.
Occupational exposures
Exposure to workplace dusts found in coal mining, gold mining, and the cotton textile industry and chemicals such as cadmium, and fumes from welding have been implicated in the development of airflow obstruction. Exposure of these irritants causes the airway to be hyper responsive.
Infection
Infections is risk factor for developing COPD. Severe recurring respiratory tract infection in childhood have been associated with reduced lung function and increased respiratory symptoms in adulthood. Recurring infections impair normal defense mechanisms, making bronchioles and alveoli more susceptible to injury.
Genetics-Alpha 1-antitrypsin deficiency is a genetic condition-
Genetics-Alpha 1-antitrypsin deficiency is a genetic condition that is responsible for about 2% of cases of COPD. In this condition, the body does not make enough of a protein, alpha 1-antitrypsin. Alpha 1- antitrypsin protects the lungs from damage caused by protease enzymes, such as elastase and trypsin, that can be released as a result of an inflammatory response to tobacco smoke.
CLINICAL FEATURES
- Chronic cough
- Sputum production
- Wheezing
- Chest tightness
- Dyspnoea on exertion
- Wt. loss
- Respiratory insufficiency
- Respiratory infections
- Barrel chest- chronic hyperinflation leads to loss of lung elasticity.
Bronchitis
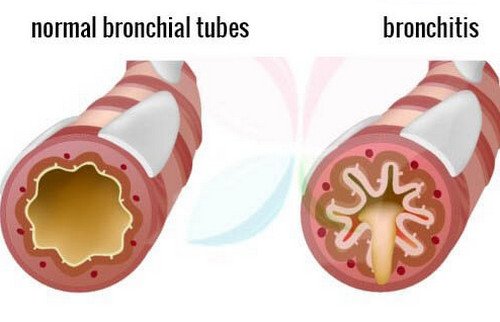
- Bronchitis results from inflammation of bronchi leading to increased mucus production, cough and eventual scaring of the bronchial lining.
- Acute (short term) Infections or lung irritants cause acute bronchitis.
- Chronic is an ongoing, serious condition. It occurs if the lining of the bronchial tubes is constantly irritated and inflamed, causing a long-term cough with mucus
- It is defined as the presence of cough and sputum production for at least 3 months.
Chronic bronchitis is characterized by the following
- An increased in size and number of submucous glands in the large bronchi, which increase mucus production.
- An increased number of goblet cells which also secrete mucus.
- Impaired ciliary function which reduce mucus clearance.
PATHOPHYSOPLOGY
- Irritants irritate the airway
- Excess mucus production
- Inflammation
- Cause the mucus secreting glands and goblet cells to increase in number.
- Ciliary function is reduced
- More mucus production
- Bronchial walls become thickened and lumen narrows and mucus plug the airway
- Alveoli adjacent to the bronchioles may become damaged and fibrosis.
- Alter function of alveolar macrophages.
- Infection
Signs and symptoms-Acute
- Sore throat,
- Fatigue (tiredness),
- Fever, body aches,
- Stuffy or runny nose,
- Vomiting, and
- Diarrhoea
- Persistent cough
- Cough may produce clear mucus
- Shortness of breath
Chronic symptoms
- Coughing,
- Wheezing, and
- Chest discomfort.
- The coughing may produce large amounts of mucus. This type of cough often is called a smoker's cough.
EMPHYSEMA
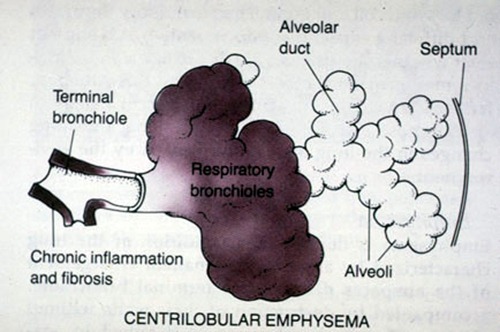
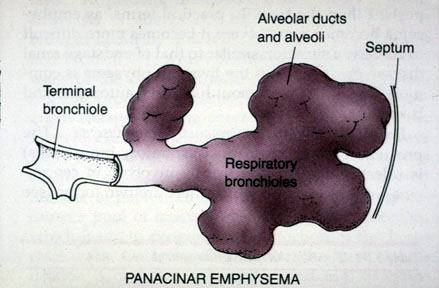
- Definition- Emphysema is defined as enlargement of the air spaces distal to the terminal bronchioles, with destruction of their walls of the alveoli.
- As the alveoli are destroyed the alveolar surface area in contact with the capillaries decreases. Causing dead spaces (no gas exchange takes place) Leads to hypoxia.
In later stages
CO2 elimination is disturbed and increase in CO2 tension in arterial blood causing respiratory acidosis
There are three types of emphysema
- Centriacinar
- Panacinar
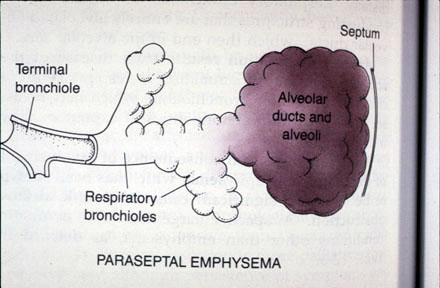
- Paraseptal
Centriacinar (centrilobular) emphysema the most common type produce destruction in bronchioles usually in the upper lung region. Inflammation begins in the bronchioles and spread peripherally but usually the alveolar sac remains intact. This form of emphysema occurs most often in smokers.
Panacinar emphysema destroys the entire alveolus and most commonly involves the lower portion of the lung. This form of disease is generally observed in individuals with ATT (Alpha-1 antitrypsin deficiency) deficiency.
Paraseptal or distal acinar emphysema primarily involves the distal airway structures alveolar ducts and alveolar sacs. The process is localized around the septa of the lung or pleura. It is believed to be the likely cause of spontaneous pneumothorax.
DIAGNOSIS
Clinical Assessment
Blood Test
- CBC
- ESR
Blood tests can help determine if symptoms are being caused by an infection.
An arterial blood gas test will measure the amount of oxygen in blood. This is one indication of how well lungs are working. This can help doctor determine how severe COPD is and whether need oxygen therapy.
Chest X-ray or CT scan
A CT scan is a type of X-ray that creates a more detailed image than a standard X-ray. Whichever type doctor chooses, an X-ray will give a picture of the structures inside chest. These include your heart, lungs, and blood vessels. Your doctor will be able to see if client has evidence of COPD. If symptoms are being caused by another condition such as heart failure, the doctor will be able identify that as well.
Sputum Examination
Doctor may order a sputum examination, especially if the client has a productive cough. Sputum is the mucus the client cough up. Analyzing sputum can help identify the cause of breathing difficulties and may rule out some lung cancers. If there is a bacterial infection, it can be identified and treated.
ECG
The doctor might request an ECG to determine if your shortness of breath is being caused by a heart condition.
Pulmonary Function Test
- Pulmonary function tests (PFTs) measure how well the lungs are moving air in and out. They also measure how well the lungs are moving oxygen to the blood.
- Spirometry (meaning the measuring of breath) is the most common of the pulmonary function tests (PFTs). It measures lung function, specifically the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled.

MANAGEMENT
- MEDICAL MANAGEMENT
- SURGICAL MANAGEMENT
- NURSING MANAGEMENT
MEDICAL MANAGEMENT
The treatment goal for the client with COPD are
- To improve ventilation
- To facilitate the removal of bronchial secretions
- To promote health maintenance
- To reduce complications, and
- To slow progression of the disease
Bronchodilator drug therapy are agents that widen the air passages by relaxing the bronchial smooth muscle and improve the ventilation of lungs. They are usually administered via inhalation route but in rare occasions may be given orally or administered intravenously. Regular treatment with long acting bronchodilators' is more effective and convenient than treatment with short acting forms.
Phosphodiesterase-4 (PDE-4) Inhibitor
A new drug called roflumilast (Dalliers) can help with severe COPD symptoms
It brings down swelling in the Lungs and opens up your airways. You might take it with a long-acting bronchodilator. Side effects include Diarrhea and weight loss.
Theophylline
Theophylline can help your lungs work better, but it may not control all of your symptoms.
Steroids
These bring down swelling in your airways. You usually breathe them in through an inhaler.
- Budesonide and formoterol
- Fluticasone and salmeterol
- The principal bronchodilator treatment is Beta2 agonists, anticholinergics, and methylxanthines used singly or combination. The choice of bronchodilators depends on availability and patient’s response.
- Short acting Beta2 agonists (e.g., albuterol) have minimal adverse effects with rapid onset of action, a peak effect in 60 to 90 minutes and duration of 4 to 6 hour.
- Side effects that may develop with the use of these drugs are tachycardia, tremor, nervousness, and nausea.
- Anticholinergic agents offer greater bronchodilator effect and fewer side effect than short acting inhaled beta2 agonists.
Oxygen therapy O2 therapy is frequently used in the treatment of COPD another problem associated with hypoxemia.
Indications for us: Goals for 02 therapy are
- To reduce the work of breathing,
- To maintain the PaO2
- To reduce the workload of heart
To keep the SaO2 more than 90% during rest
Lifestyle Changes
A few changes to your daily life can also help you breathe easier.
Talk to a dietitian
You might need to eat smaller meals more often or take supplements to get the nutrients you need.
Exercise
This is also important when you have COPD. It strengthens the muscles that help you breathe.
SURGICAL MANAGEMENT
Bullectomy
Bullae are enlarged airspaces that do not contribute to ventilation but occupy space in the thorax, these areas may be surgically excised
lung volume reduction surgery
It involves the removal of a portion of the diseased lung parenchyma. this allows the functional tissue to expand. lung transplantation- is a surgical procedure in which a patient's diseased lungs are partially or totally replaced by lungs which come from a donor.
Nursing theory model of Rosenstock & Becker’s Health Belief Model
According to Fundamentals of Canadian Nursing, Rosenstock and Becker’s Health Belief Model is constructed with the assumption that a health-related action depends on the simultaneous occurrence of three factors-
- Enough motivation to prioritize health,
- Vulnerability or susceptibility to serious health problems and their accompanying consequences, and
- The ideology that following health care advice is beneficial.

DISEASE CONDITION-CHRONIC OBSTRUCTIVE PULMONARY
- Individual perception
- Shortness of breath
- Dyspnoea
- Coughing
- sore throat
Perceived Seriousness of COPD
- Respiratory Failure
- Congestive Heart Failure
- Atelectasis lung
- Cardiac Arrest
- Deaths
2. Modifying Factors
- Age of patient
- Education
- Occupation
- Recurrent attacks of Disease and admission of patient
Perceived threat of COPD measure by Nurses Knowledge and practise through check-up and structured Questionnaire
3. Likelihood of Action
- Preventive measure adopted by patient
- Stop smoking.
- Avoid secondhand smoke.
- Avoid air pollution.
- Avoid occupational exposures.
- Know your family history.
B. Use of Nebulization
- Counselling of the patient
- Regular use of Medication
- Regular Health Check-ups
Complications
- More frequent lung infections, such as pneumonia.
- An increased risk of thinning bones (osteoporosis), especially if you use oral corticosteroids.
- Problems with weight. If chronic bronchitis is the main part of your COPD.
- Heart failure affecting the right side of the heart
- Lung cancer
- A collapsed lung (pneumothorax).
- Sleep problems.
- Depression.
Nursing management
1. Nursing diagnosis
Impaired gas exchange related to decreased ventilation
Objectives
Improve ventilation
Intervention
- Monitor lung sounds every 4 to 8 hours.
- Perform chest physiotherapy
- Advice the client to drink at least 8 to 10 glasses of fluid per day unless contraindicated
- Teach the client in coughing technique
- Asses the condition of oral mucus membrane and perform oral care
- Nursing diagnosis
Disturbed sleep pattern related to dyspnoea
Objectives
Getting adequate rest
Intervention
- Promote relaxation by providing a darkened, quiet environment, ensure adequate room ventilation.
- Avoid use of sleeping pills
- Schedule care activities to allow periods of uninterrupted sleep.
- Nursing diagnosis
Activity intolerance related to inadequate oxygenation
Objective
Improve to perform daily activity
Intervention
- Monitor the severity of dyspnea
- Stop or slow any activity that leads to change in respiratory rate
- Advice the client to avoid conditions that increase oxygen demand
- Nursing diagnosis
Anxiety related to acute breathing difficulties and fear of suffocation
Objectives
Relieve fear of dying
Intervention
- Provide a quiet, calm environment.
- During acute episodes, open doors and curtains and limit the number of people in the room.
- Encourage the use of breathing retraining and relaxation technique
- Give sedative and tranquilizers with extreme caution.
- Nonpharmacological
- Nursing diagnosis
Ineffective airway clearance related to excessive secretions and ineffective coughing
Objective
Effective airway clearance
Intervention
- Monitor lung sounds every 4 to 8 hours.
- Perform chest physiotherapy
- Advice the client to drink at least 8 to 10 glasses of fluid per day unless contraindicated
- Teach the client in coughing technique
- Asses the condition of oral mucus membrane and perform oral care