Anaesthesia in Obstetrics
Anaesthesia
"Anesthesia" means loss of feeling, either by way of "going to sleep" (general anesthesia) or just Numbing an area or region of the body (for example, epidural anesthesia)
Types of Obstetric Anesthesia
- Epidural- Epidurals are commonly used during childbirth to help manage the mother’s pain.
- Spinal Block. Similar to an epidural, a spinal block may be used on the lower back to desensitize the area.
- Pudendal Block. To relieve pain of the vagina and rectum before a child is born, a Pudendal block may be given.
- Combined Spinal-Epidural. For those that want the quickness of a spinal block in combination.
Local Anesthetic Agents in Obstetrics-
|
Drug |
Usual Dose | Onset | Duration | Use in Obstetrics |
| Lignocaine | 7 mg/kg | Rapid | 60–90 min | Local or pudendal block and also for epidural or spinal for cesarean delivery |
| Bupivacaine | 3 mg/kg | Slow | 90–150 min | Epidural or spinal for cesarean delivery |
REGIONAL ANESTHESIA
When complete relief of pain is needed throughout labor, epidural analgesia is the safest and simplest method for procuring it. It provides sensory as well as various degrees of motor blockade over a region of the body. But anesthetists/obstetricians have to be trained properly to make use of this very valuable method in normal and abnormal labor.

Advantages of Regional
Anesthesia
- The patient is awake and can enjoy the birth time
- CSE allows women to move
- Newborn Apgar score generally good
- Lowered risk of maternal aspiration
- Postoperative pain control is better.
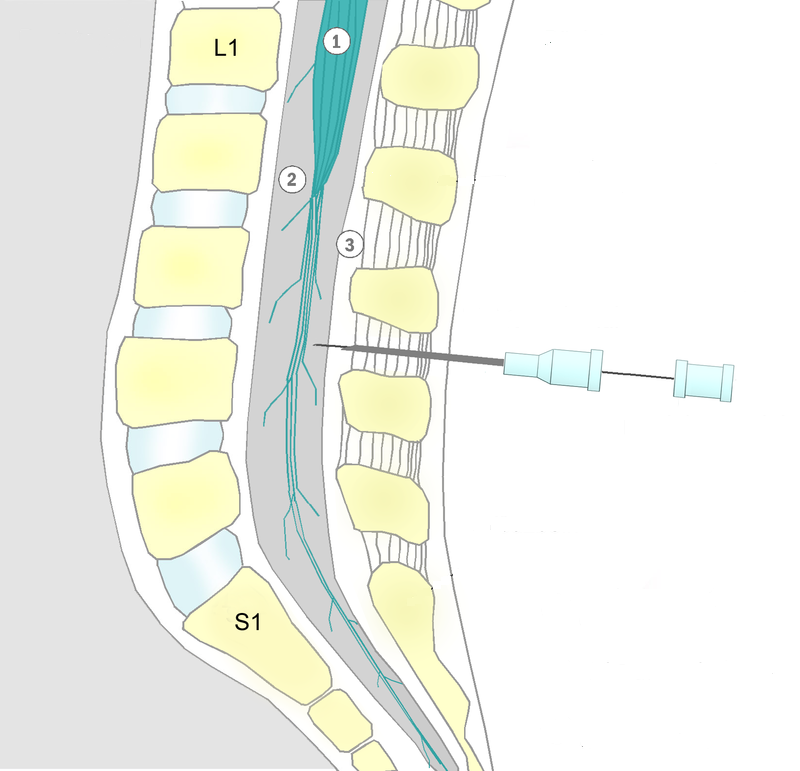
Continuous Lumbar Epidural Block-
A lumbar puncture is made between L2 and L3 with the epidural needle. With the patient on her left side, the back of the patient is cleansed with antiseptics before injection. When the epidural space is ensured, a plastic catheter is passed through the epidural needle for continuous epidural analgesia. A local anesthetic agent (0.5% bupivacaine) is injected into the epidural space. Full dose is given after a test dose when there is no toxicity. For complete analgesia a block from T10 to the S5 dermatomes is needed. For cesarean delivery a block from T4 to S1 is needed.
Epidural analgesia is especially beneficial
- Pregnancy-induced hypertension,
- Breech presentation
- Twin pregnancy and preterm labor.
- Previous cesarean section is not a contraindication.
- Epidural analgesia when used there is no change in duration of first stage of labor. But second stage of labor appears to be prolonged by 15–30 minutes. This might lead to frequent need of instrumental delivery like forceps or ventouse.
| Contraindications | Complications |
| Maternal coagulopathy or anticoagulant therapy | Hypotension due to sympathetic blockade |
| Supine hypotension | Pain at the insertion site. Back pain |
| Hypovolemia | Post spinal headache due to leakage of cerebroapinal fluid through the needle hole in the Dura |
| Neurological diseases | Total spinal due to inadvertent administration of the drug in the subarachnoid space. |
| Spinal deformity or chronic low back pain | Injury to nerves, convulsions, Pyrexia |
| Skin infection at the injection site | Ineffective analgesia |
Paracervical Nerve Block-
- Is useful for pain relief during the first stage of labor. Following the usual antiseptic safe guards
- A long needle (15 cm or more) is passed into the lateral fornix, at the 3 and 9 o’clock positions.
- Five to ten milliliters of 1% lignocaine are injected at the site of the cervix and the procedure is repeated on the other side.
- This dose is quite sufficient to relieve pain for about an hour or two, and injections can be given more than once if necessary.
- Bupivacaine is avoided due to its cardiotoxicity. Paracervical block should not be used where placental insufficiency is present
- Although paracervical block may be used from 5 cm dilatation of the cervix, it is most useful toward the end of the first stage of labor to remove the desire to bear down earlier.
- Paracervical block can only relieve the pain of uterine contraction and the perineal discomfort is removed by pudendal nerve block.
- Fetal bradycardia is a known complication. This is due to decreased placental perfusion resulting from uterine artery vasoconstriction.
- This method is not commonly used.

Pudendal Nerve Block-
- It is a safe and simple method of analgesia during delivery. Pudendal nerve block does not relieve the pain of labor but affords perineal analgesia and relaxation.
- Pudendal nerve block is mostly used for forceps and vaginal breech delivery.
- This method of analgesia is associated with less danger, both for mother and baby than general anesthesia.
- Technique- The pudendal nerve may be blocked by either the transvaginal or the trans perineal route.

Transvaginal Route-
- Transvaginal route is commonly preferred. A 20 mL syringe, one 15 cm (6”) 22gauge spinal needle and about 20 mL of 1% lignocaine hydrochloride are required.
- The index and middle fingers of one hand are introduced into the vagina, the finger tips are placed on the tip of the ischial spine of one side.
- The needle is passed along the groove of the fingers and guided to pierce the vaginal wall on the apex of ischial spine and thereafter to push a little to pierce the sacrospinous ligament just above the ischial spine tip. After aspirating to exclude blood, about 10 mL of the solution is injected.
- The similar procedure is adopted to block the nerve of the other side by changing the hands.Complications:
Hematoma formation, Infection and rarely intravascular injection or allergic reaction. Toxicity may affect-
- CNS- Excitation, ringing in the ears and convulsions.
- Cardiovascular- Tachycardia, Hypotension, Arrythmias, even Cardiac arrest.
Spinal Anesthesia
- Spinal anesthesia is obtained by injection of local anesthetic agent into the subarachnoid space.
- It has less procedure time and high success rate.
- Spinal anesthesia can be employed to alleviate the pain of delivery and during the third stage of labor. For normal delivery or for outlet forceps with episiotomy, ventouse delivery, block should extend from T10 (umbilicus) to S1. For cesarean delivery level of sensory block should be up to T4 dermatome.
- Spinal anesthesia can be obtained by injecting the drug into the subarachnoid space of the third or fourth lumbar interspace.
- The patient lying on her side with a slight head up tilt. The blood pressure and respiratory rate should be recorded every 3 minutes for the first 10 minutes and every 5 minutes thereafter.
- Oxygen should be given for respiratory depression and hypotension.
- It is used during vaginal delivery, forceps, ventouse and cesarean delivery
Side Effects of Spinal Anaesthesia
- Hypotension due to blocking of sympathetic fibers leading to vasodilatation and low cardiac output
- Respiratory depression may occur due to paralysis of respiratory muscles including diaphragm (C3 –C5)
- Failed block, chemical meningitis, epidural abscess
- Total spinal—due to excessive dose or improper positioning
- Post spinal headache—due to low or high CSF pressure and leakage of CSF
- Meningitis due to faulty asepsis
- Transient or permanent paralysis
- Toxic reaction of local anesthetic drugs
- Paralysis and nerve injury
- Nausea and vomiting are not uncommon
- Urinary retention (bladder dysfunction)
The advantages of spinal anesthesia are:
- less fetal hypoxia unless there is hypotension
- Minimal blood loss.
- The technique is not difficult and no inhalation anesthesia is required, but post spinal headache occurs in 5–10% of patients.
Combined spinal-epidural analgesia (CSE):
- An introducer needle is first placed in the epidural space.
- A small gauge spinal needle is introduced through the epidural needle into the subarachnoid space (needle through needle technique).
- A single bolus of 1 mL 0.25% bupivacaine with 25 μg fentanyl is injected into the subarachnoid space.
- The spinal needle is then withdrawn.
- An epidural catheter is thus sited for repeated doses of anesthetic drug.
- The method gives rapid and effective analgesia during labor and cesarean delivery.
- It allows women to move (walking epidural) during labor.
INHALATION METHODS
- Premixed nitrous oxide and oxygen- Cylinders contain 50% nitrous oxide and 50% oxygen mixture. Entonox apparatus has been approved for use by midwives. This agent is used in the second phase (from 8 cm dilatation of cervix to delivery). It can be self administered. Entonox is most commonly used inhalation agent during labor in the UK. Hyperventilation, dizziness, hypocapnia are the side effects. The woman is to take slow and deep breaths before the contractions and to stop when the contractions are over. The woman should be monitored with pulse oximetry.
GENERAL ANESTHESIA FOR CESAREAN SECTION
The following are the important considerations-
- Cesarean section may have to be done either as an elective or emergency procedure
- Ryle's tube aspiration of gastric contents is to be done, especially when the stomach contains food materials
- A large number of drugs pass through the placental barrier and may depress the baby
- Uterine contractility may be diminished by volatile anesthetic agents like ether, halothane
- Halothane, Isoflurane cause cardiac depression, hepatic necrosis and hypotension
- Hypoxia and hypercapnia may occur
- Time interval from uterine incision to delivery is related directly to fetal acidosis and hypoxia
- Longer the exposure to general anesthetic before delivery the more depressed is the Apgar score.
Preoperative Preparations:
These safety measures should be taken to prevent complications of general anesthesia-
- Preoperative medication with sedatives or narcotics is not required as they cause respiratory depression of the fetus.
- Fasting of about 6 hours is preferable for an elective surgery
- High-risk women in labor should preferably not be allowed to eat.
- Ryle's tube aspiration of gastric contents is to be done when the stomach contains food materials
- H2 -blocker (Ranitidine 150 mg orally) should be given night before (elective procedure). H2 receptor blocking agent and metoclopramide is to be given IM especially to women with high risks (obesity).
- Non-particulate antacid (0.3 molar sodium citrate 30 mL) is given orally before transferring the patient to theater to neutralize the existing gastric acid
- While on the theater table, left lateral tilt of the woman is maintained with a wedge on the back. This is to avoid Aortocaval compression as it is detrimental to both mother and fetus.
- Metoclopramide (10 mg IV) is given after minimum 3 minutes of preoxygenation to decrease gastric volume and to increase the tone of lower esophageal sphincter.
- Intubation with adequate cricoid pressure. A technique used in endotracheal intubation to try to reduce the risk of regurgitation.
Important Points-
- Commonly used Antihypertensive in pregnancy are- Methyldopa, labetalol, Hydralazine and Nifedipine. Hydralazine, Labetalol.Nitroglycerine and sodium nitroprusside and used for Hypertensive crisis.
- Commonly used tocolyties are- Calcium channel blockers, magnesium sulfate, oxytocin antagonists and nitric oxide donors, betamimetics (terbutaline ritodrine,isoxsusprine., indomethacin.
- Tocolytics are used to delay preterm labor for a short-term period (48 hours). Delay in delivery for 48 hours is for corticosteroids. to work and to allow intrauterine transfer of the fetus to a center equipped with NICU facilities. Side effects and the precautions of use must be known.
-
Anticonvulsants used in pregnancy are- Magnesium sulfate, diazepam and phenytoin. MgSO4, is the drug of choice in eclampsia.
-
While breastfeeding, the benefits of breastmilk must be weighed against the risk drug exposure to the neonate, Information
as regards some commonly used drugs are available. -
Teratogens exert their effects through different mechanisms. The hazards of drugs depend upon the placental transfer of drugs and the period of gestation.
-
Opioid analgesics are commonly used in labor. They work primarily as a sedative. Of the inhalation methods, premixed nitrous oxide and oxygen are commonly used.
-
Epidural analgesia is the safe, effective and simple method of regional anesthesia. One must know the contraindications and complications of its use. In obstetrics, it is especially beneficial for some cases.
-
Pudendal block is good for perineal analgesia and is used for forceps and vaginal breech delivery.
-
Spinal anesthesia has some advantages but it should be used carefully to avoid the side effects.
-
Mendelson's syndrome is a serious complication of general anesthesia. this can be prevented when the safety measures are taken beforehand.
-
Mendelson's syndrome, named in 1946 for American obstetrician and cardiologist Curtis Lester Mendelson, is a form of chemical pneumonitis or aspiration pneumonitis caused by aspiration of stomach contents (principally gastric acid) during anaesthesia in childbirth.