Unconsciousness
Consciousness
- A state of awareness of yourself and your surroundings
- Ability to perceive sensory stimuli and respond appropriately to them.
Unconsciousness-A state of complete or partial unawareness or lack of response to sensory stimuli. Various degrees of unconsciousness are there: e.g. confusion, stupor, somnolent, excitary and deep coma etc
Abnormal state - client is unarousable and unresponsive.
- Coma is a deepest state of unconsciousness.
- Unconsciousness is a symptom rather than a disease.
Degrees of unconsciousness that vary in length and severity:
- Brief -Fainting
- Prolonged - Deep coma
Causes of unconsciousness
- Trauma
- Epidural / Subdural hematoma
- Brain contusion
- Hydrocephalus
- Stroke
- Tumor
- Infection
- Meningitis
- Encephalitis
- Hypo/hyperglycemia
- Hepatic encephalopathy
- Hyponatremia
- Drug /alcohol overdose
- Poisoning /intoxication
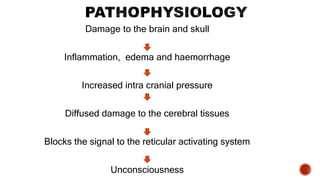
Pathophysiology
- Consciousness is a complex function controlled by reticular activating system (RAS) and its integrated components.
- The RAS begins in the medulla as the reticular formation that connects to the RAS (located in the mid-brain which then connects hypothalamus and thalamus).
- Integrated pathways connect to the cortex via the thalamus and to the limbic system via the hypothalamus. Feedback systems also connect at the brainstem level.
- The reticular formation produces wakefulness, whereas the RAS and higher connections are responsible for awareness of self and the environment.
- To produce a coma, a disorder must affect both cerebral hemisphere and the brain stem itself (in one of the three ways)
Stages of Unconsciousness
- Confusional state
- Delirium
- Obtundation
- Stupor
- Coma
1. Confusional State-Confusion is a state in which the patient cannot take into account all elements of his/her immediate environment, implying an element of sensorial clouding.
- Disoriented.
- Shortened attention span.
- Memory deficits.
- Difficulty in following commands.
- Alteration in perception of stimuli.
2. Delirium-It is characterized by a fluctuating disturbance in consciousness and change in cognition that usually develops over a short period of time.
- Disoriented to place and person.
- Increased motor activities.
- Illusion, Hallucinations
3.Obtundation-Decreased alertness and hypersomnia.
- Obtundation is characterized by reduced alertness and hypersomnia.
- Hypersomnia is technically defined as a state of sleep in excess i.e, 25% more of the expected normal sleep.
- Obtundation is often seen with substance abuse in the form of narcotic or alcohol over dosage.
4. Stupor-Stupor is unresponsiveness from which the patient can only be aroused by vigorous repeated painful stimuli.
- Deep sleep or unresponsiveness
- Can be aroused only with painful stimuli.
- Responds by withdrawing or Grabbing at the source of pain.
5.Coma- State in which a patient is totally unaware of both self and external surrounding, and unable to respond meaningfully to external stimuli.
Characteristics of coma
- No eye-opening
- Inability to follow instructions
- No speech or other forms of communication
- No purposeful movement
Sign and Symptom
- The person will be unresponsive (does not respond to activity, touch, sound, or other stimulation
- Is unaware of his surroundings and does not respond to sound
- Makes no purposeful movements
- Does not respond to questions or to touch
- Drowsiness
- Inability to speak or move parts of his or her body
- Loss of bowel or bladder control (incontinence)
- Stupor
- Respiratory changes (cheyne stroke respiration, cluster breathing, ataxic breathing, hyperventilation)
- Abnormal pupil reactions
Diagnostic test
- X-ray
- MRI (magnetic resonance imaging) -Tumors, vascular abnormalities, IC bleed
- CT (computerized tomography) - Cerebral edema, infarctions, hydrocephalus
- Lumbar puncture -Cerebral meningitis, CSF evaluation
- PET (positron emission tomography)
- EEG- electric activity of cerebral cortex
- Blood test like CBC, LFT, RFT, ABG etc.
Complications of immobility
- Skin - Pressure sore, laceration.
- Respiratory- Hypostatic pneumonia, pulmonary Embolism.
- C.V. complications - DVT(Deep Vein Thrombosis), postural hypotension, thrombo embolism.
- G.I. system - Paralytic ilius, constipation, distention.
- Urological - UTI, stone.
- Muskulo skeleton- Contracture, osteoporosis, dystrophy, weakness.
- Neurological - Foot drop.
- Psychological - Anxiety, depression
Medical Management
The goal of medical management are to preserve brain function and prevent further damage.
- Ventilatory support
- Oxygen therapy
- Management of blood pressure
- Management of fluid balance
- Management of seizures -anti epileptic sedatives, paralytic agents
- Treating Increased ICP -Mannitol, corticosteroids
- Management of temperature regulation (fever)- ice packs, tepid sponging, Antipyretics, NSAIDS
- Management of elimination - laxatives
- Management of nutrition- TPN (total parental nutrition) and RT feeds
- DVT prophylaxis
Nursing Diagnosis
- Ineffective airway clearance related to altered level of consciousness.
- Risk for injury related to decreased level of consciousness.
- Risk for impaired skin integrity related to immobility.
- Impaired urinary elimination related to impairment in sensing and control.
- Disturbed sensory perception related to neurologic impairment.
- Interrupted family process related to health crisis.
- Risk for impaired nutritional status
Nursing management of unconscious patient (emergency care)
A. Maintaining a patent airway
- ABC Management
- ABG results must be interpreted to determine the degree of oxygenation provided by the ventilators or oxygen.
- Assess for cough and swallow reflexes
- Use an oral artificial airway to maintain patency
- Tracheotomy or endo-tracheal intubation and mechanical ventilation maybe necessary Preventing airway obstruction
- Oronasopharyngeal suction equipment may be necessary to aspirate secretions.
- If facial palsy or hemi paralysis is present the affected side must be kept the uppermost.
- Dentures are removed
- Nasal and oral care is provided to keep the upper airway free of accumulated secretions debris
- Monitoring neurological signs at intervals determined by their condition and document results.
B. Ineffective Cerebral tissue Perfusion
- Assess the Glasgow Coma Scale(GCS) SPO2 level and Arterial blood gas (ABG) of the patient.
- Monitor the vital signs of the patients (increased temperature)
- Head elevation of 30 degrees, neutral position maintained to facilitate venous drainage. Reduce agitation .(Sedation.)
- Reduce cerebral edema (Corticosteroids, osmotic or loop diuretics.) Generally peaks within 72 hrs after trauma and subsides gradually.
- Talk softly and limit touch and stimulation.
- Administer laxatives, and antiemetic as ordered
- Manage temperature with antipyretics and cooling measures.
- Prevent seizure with ordered dilantin.
- Administer mannitol 25-50 g IV bolus if ICP >20, as prescribed.
C. Risk for increased ICP
- Head elevation of 30 degrees, neutral position maintained to facilitate venous drainage and prevent aspiration.
- Pre-oxygenation before suctioning should be mandatory , and each pass of the catheter limited to 10 seconds, with appropriate sedation to limit the rise in ICP.
- Insertion of an oral airway to suction the secretions.
- As fluid intake is restricted and glucose is avoided to control cerebral edema and intravenous infusion cannot be considered as a nutritional support.
Nursing management of unconscious patient (routine care)
A. Fluid and electrolyte balance
- Intake-Output chart should be meticulously maintained.
- Assess and document symptoms that may indicate fluid volume overload or deficit. Diuretics may be prescribed to correct fluid overload and reduce edema.
- Over hydration and intravenous fluids with glucose are always avoided in comatose patients as cerebral edema may follow.
B. Skin integrity
- The nurse should provide intervention for all self-care needs including bathing, hair care, skin and nail care.
- Frequent back care should be given.
- Comfort devices should be used.
- Positions should be changed.
- Special mattresses or airbeds to be used.
- Adequate nutritional and hydration status should be maintained.
- Patient’s nails should be kept trimmed.
- Cornea should be kept moist by instilling methyl cellulose 0.5% to 1%.
- Protective eye shields can be applied or the eyelids closed with adhesive strips if the corneal reflex is absent. These measures prevent corneal abrasions and irritation.
- Inspect the oral cavity.
- Keep the lips coated with a water-soluble lubricant to prevent encrustation, drying, cracking. Inspect the paralyzed cheek.
- Frequent oral hygiene every 4 hourly.
- Nasal passages may get occluded so they may be cleaned with a cotton tipped applicator.
C. Proper positioning
- Lateral position on a pillow to maintain head in a neutral position
- Upper arm positioned on a pillow to maintain shoulder lignment
- Upper leg supported on a pillow to maintain alignment of the hip
- Change position to lie on alternate sides every 2-4hrs
- Taking care to prevent injury to soft tissue and nerves, edema or disruption of the blood supply
- Maintaining correct positioning enables secretions to drain from the client’s mouth, the tongue does not obstruct the airway and postural deformities are prevented.
D. Self care deficit
- Attending to the hygiene needs of the unconscious patient should never become ritualistic, and despite the patient's perceived lack of awareness, dignity should not be compromised.
- Involving the family in self care needs.
- Fingernails and toenails also need to be assessed
- Chronic illnesses, such as diabetes needs more attention
- Minimum two nurses should bathe an unconscious patient as turning the patient may block the airway.
- Proper assessment of the condition of the skin must be done when giving a bed bath. Hair care should not be neglected.
E. Oral Hygiene
- A chlorhexidine based solution is used.
- Airway should be removed when providing oral care. It should be cleaned and then re-inserted.
- If the patient has an endotracheal tube the tube should be fixed alternately on each side.
- Minimum of four-hourly oral care to reduce the potential of infection from micro-organisms.
- Also not to damage the gingiva by using excessive force.
F. Eye Care
- In assessing the eyes, observe for signs of irritation, corneal drying, abrasions and oedema.
- Gentle cleaning with gauze and 0.9% sodium chloride should be sufficient to prevent infection.
- Artificial tears can also be applied as drops to help moisten the eyes.
- Corneal damage can result if the eyes remain open for a longer time.
- Tape can be used to close the eyes
G. Nutrition need
- TPN (Total parenteral nutrition)
- Enteral feeding via Nasogastric, nasojejunal or PEG tube.
- Intravenous fluids are administered for comatose patients.
H. Risk for injury
- Side rails must be kept whenever the patient is not receiving direct care.
- Seizure precautions must be taken.
- Adequate support to limbs and head must be given when moving or turning an unconscious patient.
- Protect from external sources of heat.
- Oversedation should be avoided – as it impedes the assessment of the level of consciousness and impairs respiration.
- Assess the Need for restrain.
I. Impaired bowel/ bladder functions
- Assess for constipation and bladder distention.
- Auscultate bowel sounds.
- Stool softeners or laxatives may be given.
- Bladder catheterization may be done.
- Catheter care must be provided under aseptic techniques.
- Monitor the urine output and colour.
- Initiate bladder training as soon as consciousness has regained.
j. Risk for contractures
- Maintain the extremities in functional positions by providing proper support.
- Remove the support devices every four hours for passive ROM(Range of motion) exercises and skin care.
- Foot support should be provided.
K. Sensory stimulation
- Brain needs sensory input.
- Widely believed that hearing is the last sense to go.
- Talk, explain to the patient what is going on.
- Upon waking many clients remember….. and will accurately recall events and processes that happened while they were “sleeping”(unconscious)
L. Nurses must
- Show respect.
- Encourage family to contribute to the care of their loved ones.
- Afford the privacy both the client and family deserve.
M. Encourage stimulation by
- Massage
- Combing/washing hair
- Playing music/radio/CD/TV
- Reading a book
- Bring in perfumed flowers
- Update them with family news
N. Impaired family process
- Include the family members in patient’s care.
- Communicate frequently with the family members.
- The family members should be allowed to stay with the patient when and where it is possible.
- Use external support systems like professional
- Counsellors, religious clergy etc.
- Clarifications and questions should be encouraged