RUHS BSc Nursing 1 Semester APPLIED ANATOMY & APPLIED PHYSIOLOGY Main Examination November 2023
28-11-2023 B.Sc. Nursing-1 Semester (Main) Examination November-2023
5001
APPLIED ANATOMY & APPLIED PHYSIOLOGY
Instructions to the candidates:
- Do not write anything on question paper except Rall Number, otherwise it shall be deemed as an act of indulging in unfair means and action shall be taken as per rules.
- Use separate answer book for each section,
Duration: 3 Hours Total Marks: 75
Section-A (Applied Anatomy)
1. Long/Essay type questions (Attempt any one): 1 x 10=10
- Describe chambers, layers and coronary circulation of heart.
- Describe gross anatomy of liver and explain flow of bile.
2. Short notes (Attempt any three): 3x5=15
- Structure of pancreas
- Classification of joints with example
- Muscles of upper limb
- Blood supply of kidney
3. Very short questions (Attempt any three): 3x2=6
- Structure of neuron
- Clinical significance of prostate gland
- Layers of uterus
- Labes of lungs
4. Answer the following MCQ: 6x1=6
i) The left common carotid artery arises from:
- Brachiocephalic artery
- Ascending aorta
- Descending aorta
- Arch of Aorta
li) The largest lymph organ is:
- Tonsils
- Thymus gland
- Spleen
- Liver
lii) Which nerve supplies the diaphragm?
- Phrenic
- Pudendal
- Intercostal
- Sciatic
iv) The common bile duct is form by fusion of:
- Right and left hepatic duct
- Cystic and right hepatic duct
- Cystic and left hepatic duct
- Cystic and common hepatic duct
v) Bones that forms knee joint are:
- Radius, Ulna, Femur
- Tibla, Fibula, Femur
- Tibia, Femur, Patellab
- Radius, Femur, Patella
vi) Choose correct option for external urethral sphincter:
- Striated muscles & voluntary
- Striated muscles & Involuntary
- Smooth muscles & voluntary
- Smooth muscles & Involuntary
Section-B (Applied Physiology)
1. Long/Essay type questions (Attempt any one): 1x10=10
- Explain mechanism of respiration in detail.
- Describe name, functions and diseases caused by alteration of adrenal gland hormones.
2. Short notes (Attempt any three): 3x5=15
- Explain cardiac cycle
- Composition and functions of saliva
- Blood group types
- Functions of skin
3. Very short questions (Attempt any three): 3x2=6
- Fertilization
- Functions of hypothalamus
- Nerve impulse conduction
- Explain GFR
4. Answer the following MCQ: 7x1=7
i) Which eye part assist in accommodation of near vision:
- Lens
- Retina
- Pupils
- Iris
ii) Thyroid stimulating hormone is secreted by:
- Anterior pituitary
- Posterior pituitary
- Thymus gland
- Thyroid gland
iii) Which of the following cranial nerve is motor?
- Olfactory
- Optic
- Trochlear
- Vagus
Iv) Thalassemia is associated with abnormal production of:
- Neutrophils
- Haemoglobin
- Thrombocytes
- Prothrombin
v) Which of the following enzyme is present in saliva?
- Pepsin
- Pepsinogen
- Amylase
- All of the above
vi) Enzyme secreted by the kidneys that is involved in control of blood pressure is:
- Erythropoietin
- Angiotensinogen
- Urobilin
- Renin
vii) Light band of sarcomere is made up of:
- Only thin filaments
- Only thick filaments
- Both thin & thick filaments
- Neither thin nor thick filaments
Section-A (Applied Anatomy)
1. Long/Essay type questions (Attempt any one): 1 x 10=10
- Describe chambers, layers and coronary circulation of heart.
Ans-
Heart
Heart is a hollow muscular organ that pumps blood throughout the circulatory system. It is situated in between two lungs in the mediastinum. It is made up of four chambers, two atria and two ventricles.
The apex is about 9 cm to the left of the midline at the level of the 5th intercostal space, i.e. a little below the nipple and slightly nearer the midline. The base extends to the level of the 2nd rib.
- Shape-Cone with Broad base and Narrow Apex
- Size (close fist)-Length-12cm
- Width-9cm
- Thickness -6cm
- Weight- Adults Male-300gram
- Adults female 250gram
Organs associated with the heart-
- Inferiorly - The apex rests on the central tendon of the diaphragm
- Superiorly - The great blood vessels, i.e. the aorta, superior vena cava, pulmonary artery and pulmonary veins
- Posteriorly - The oesophagus, trachea, left and right bronchus, descending aorta, inferior vena cava and thoracic vertebrae
- Laterally -The lungs — the left lung overlaps the left side of the heart
- Anteriorly - The sternum, ribs and intercostal muscles

Right side of the Heart-
Right side of the heart has two chambers,
- Right atrium
- Right ventricle
Right atrium is a thin walled thickness is 2-3 mm and low-pressure chamber. It has got the pacemaker known as sinoatrial node that produces cardiac impulses and atrioventricular node that conducts the impulses to the ventricles.
Right atrium receives venous (deoxygenated) blood via two large veins-
- Superior vena cava that returns venous blood from the head, neck and upper limbs
- Inferior vena cava that returns venous blood from lower parts of the body
Right atrium communicates with right ventricle through Tricuspid valve. Wall of right ventricle is thick. Venous blood from the right atrium enters the right ventricle through this valve. From the right ventricle, pulmonary artery arises. It carries the venous blood from right ventricle to lungs. In the lungs, the deoxygenated blood is oxygenated.
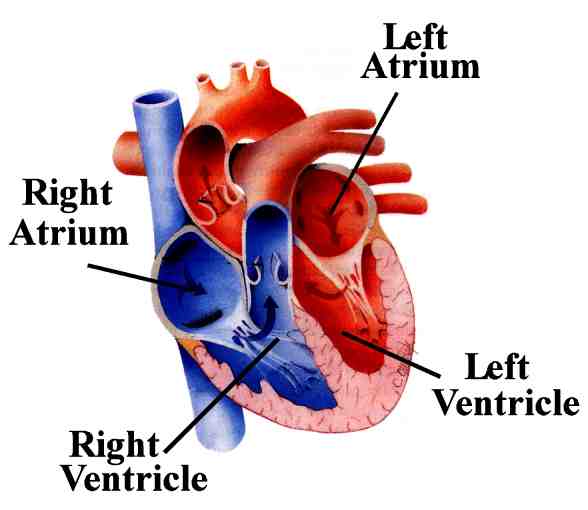
Left side of the Heart-
Left side of the heart has two chambers-
- left atrium
- left ventricle
- Left atrium is a thin walled and low-pressure chamber. It receives oxygenated blood from the lungs through pulmonary veins. This is the only exception in the body, where an artery carries venous blood and vein carries the arterial blood. Blood from left atrium enters the left ventricle through Mitral valve (bicuspid valve). Wall of the left ventricle is very thick walled thickness is 10-15 mm.
- Left ventricle pumps the arterial blood to different parts of the body through systemic aorta. and left ventricles are separated from one another by interventricular septum. The upper part of this septum is a membranous structure, whereas the lower part of it is muscular in nature.
Layers of the Heart-
Heart is made up of three layers of tissues-
- Outer pericardium
- Middle myocardium
- Inner endocardium.

A. Outer pericardium-
Pericardium is the outer covering of the heart. It is made up of two layers-
- Outer parietal pericardium
- Inner visceral pericardium.
The space between the two layers is called pericardial cavity or pericardial space and it contains a thin film of fluid.
- Outer Parietal Pericardium
Parietal pericardium forms a strong protective sac for the heart. It helps also to anchor the heart within the mediastinum.
Parietal pericardium is made up two layers-
- Outer fibrous layer
- Inner serous layer.
2. Inner Visceral Pericardium
Inner visceral pericardium lines the surface of myocardium. It is made up of flattened epithelial cells. This layer is also known as epicardium.
B. Middle myocardium-
Myocardium is the middle layer of wall of the heart and it is formed by cardiac muscle fibers or cardiac myocytes. Myocardium forms the bulk of the heart and it is responsible for pumping action of the heart.
Myocardium has three types of muscle fibers-
- Muscle fibers which form contractile unit of heart - Cardiac muscle fiber is bound by sarcolemma. It has a centrally placed nucleus. Myofibrils are embedded in the sarcoplasm. Sarcomere of the cardiac muscle has all the contractile proteins, namely actin, myosin, troponin and tropomyosin. Sarcotubular system in cardiac muscle is similar to that of skeletal muscle.
- Muscle fibers which form pacemaker- Pacemaker is structure in the heart that generates the impulses for heart beat. It is formed by pacemaker cells called P cells. Sinoatrial (SA) node forms the pacemaker in human heart.
- Muscle fibers which form conductive system- Impulses from SA node is transmitted to the atria directly. However, the impulses are transmitted to ventricles through various components of conducting system,
C. Endocardium-
This forms the lining of the myocardium and the heart valves. It is a thin, smooth, glistening membrane which permits smooth flow of blood inside the heart. It consists of single layer of squamous epithelium tissue.
Coronary Circulation
- Coronary circulation is the circulation of blood in the blood vessel of the heart muscles(myocardium).
- The coronary arteries delivers oxygen-rich blood to the myocardium.
- Cardiac vein remove the deoxygenated blood from the heart muscles.
Coronary circulation consists of
- Arterial supply
- Venous drainage
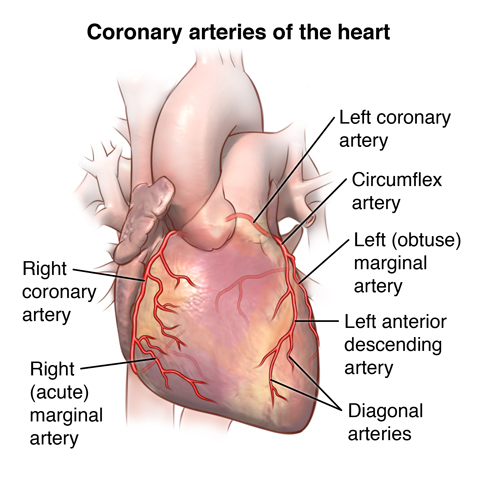
1. Coronary Arteries
- The blood flows through these arteries during diastole of heart.
- Coronary blood flow is regulated mostly by local arteriolar vasodilation in response to nutritional need of cardiac muscle.
- Diameter 1.5mm-5.2mm.
- Left coronary is larger in caliber and supplies more myocardium.
a. Right Coronary Arteries
- It arises from the right anterior aortic sinus of ascending aorta
- It passes between the right auricle and pulmonary trunk.
Branches
- Atrial branch
- Right marginal branch
- Posterior inter-venticular branch
b. Left Coronary Arteries
- It originates from left posterior aortic sinus of ascending aorta.
- It passes between pulmonary trunk and left auricle before entering the coronary sulcus.
Branches
- Anterior inter-ventricular branch(left anterior descending artery)
- Circumflex branch
Cardiac Dominance
- In about 10 % of hearts, the right coronary is rather small and is not able to give posterior inter-ventricular branch.
- In these cases, the left coronary artery provides the posterior inter-ventricular branch.
Venous Drainage- The venous drainage of the heart is by three means.
- Coronary sinus
- Anterior cardiac vein
- Venae cordis minimae
Right coronary artery supplies
- Right atrium and ventricle
- Sinu atrial and atrio-ventricular nodes
- Inter-arterial septum
- The posterior-inferior 1/3 of the inter- ventricular septum
- Posterior part of left ventricle
Left coronary arteries supplies
- Left atrium and left ventricle
- Inter-ventricular septum including atrio- ventricular bundle and its branches.
Q.1-2 Describe gross anatomy of liver and explain flow of bile.
The liver is the largest gland in the body, weighing between 1 and 2.3 kg. It is situated in the upper part of the abdominal cavity occupying the greater part of the right hypochondriac region, part of the epigastric region and extending into the left hypochondriac region.
Its upper and anterior surfaces are smooth and curved to fit the under surface of the diaphragm. its posterior surface is irregular in outline.
- Location- Right Hypochondrium, epigastrium and Left Hypochondrium
- Colour- Reddish brown
- Shape- wedge shaped
- Weight- 1.5 kg
- Both endocrine and exocrine functions
Organs associated with the liver-
- Superiorly - Diaphragm and anterior abdominal anteriorly wall
- Inferiorly - Stomach, bile ducts, duodenum, hepatic flexure of the colon, right kidney and adrenal gland
- Posteriorly - Oesophagus, inferior vena cava, aorta, gall bladder, vertebral column and diaphragm Laterally — lower ribs and diaphragm
The liver has four lobes. The two most obvious are the large right lobe and the smaller, wedge-shaped, left lobe. The other two, the caudate and quadrate lobes, are areas on the posterior surface.
The portal fissure
This is the name given to the region on the posterior surface of the liver where various structures enter and leave the gland.
The portal vein enters, carrying blood from the stomach, spleen, pancreas and the small and large intestines.
The hepatic artery enters, carrying arterial blood. It is a branch from the coeliac artery which is a branch from the abdominal aorta.
Nerve fibres, sympathetic and parasympathetic, enter here. The right and left hepatic ducts leave, carrying bile from the liver to the gall bladder.
Lymph vessels leave the liver, draining some lymph to abdominal and some to thoracic nodes.
Blood supply
The hepatic artery and the portal vein take blood to the liver. Hepatic veins, varying in number, leave the posterior surface and immediately enter the inferior vena cava just below the diaphragm.
Structure
The lobes of the liver are made up of tiny lobules just visible to the naked eye. These lobules are hexagonal in outline and are formed by cubical-shaped cells, the hepatocytes, arranged in pairs of columns radiating from a central vein. Between two pairs of columns of cells there are sinusoids (blood vessels with incomplete walls) containing a mixture of blood from the tiny branches of the portal vein and hepatic artery.
- This arrangement allows the arterial blood and portal venous blood (with a high concentration of nutrients) to mix and come into close contact with the liver cells. Amongst the cells lining the sinusoids are hepatic macrophages (Kupffer cells) whose function is to ingest and destroy any foreign particles present in the blood flowing through the liver.
- the inferior vena cava just below the diaphragm. the system of blood flow through the liver. One of the functions of the liver is to secrete bile. it is seen that bile canaliculi run between the columns of liver cells. This means that each column of hepatocytes has a blood sinusoid on one side and a bile canaliculus on the other. The canaliculi join up to form larger bile canals until eventually they form the right and left hepatic ducts which drain bile from the liver.
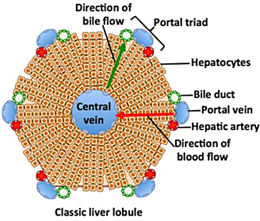
Flow of Bile
-
Bile is a bitter-tasting, dark green to yellowish brown fluid, produced by the liver.
-
Bile aids the process of digestion of lipids in the small intestine.
-
Bile is stored in the gallbladder and upon eating is discharged into the duodenum.
-
Daily secretion : 500 – 1000 ml
-
pH : 7.8 – 8.6
Secretion of Bile
Secretion occurs in three stages -
1. Formation & Secretion of constituents of bile by the liver
-
Bile salts are synthesized in hepatocytes and transferred into bile canaliculi .
-
Bile salts along with glucose, amino acids and bile pigments are actively secreted into canaliculi.
2. Filling of gall bladder-
-
Bile then passes through the biliary tree and ultimately to the hepatic duct
-
Then it reaches the gall bladder where it is concentrated and stored temporarily.
3. Discharge of bile in intestine -
-
When there is chyme in the intestine sphincter of Oddi and sphincter of Boyden are relaxed and bile flows into the intestine.
Entero hepatic circulation
-
Entero-hepatic circulation is a continuous circulation of bile salts from liver to bile and there passage into the duodenum.
-
Their absorption in the ileum and then return to the liver as a mixture of bile acids and salts.( 95% of bile salts are reabsorbed by the small intestine 5% of bile salts are lost in feces (500 - 600 mg /day)

Regulation of Bile
A. In Liver
-
Bile acid dependent - Bile secretion increases as more and more bile acids are presented to the liver by enterohepatic circulation. It occurs after fatty meal. When intestine is empty this mechanism stops.
-
Bile acid independent - It is mainly due to transfer of electrolytes by pumps(Na+ - K+ ) It is under the influence of Scretin.
B. In the Intestine -
-
Bile flows to intestine when sphincter of oddi is relaxed .
-
It is increased further due to simultaneous contraction of gall bladder and occurs in response to meal
2. Short notes (Attempt any three): 3x5=15
- Structure of pancreas
Ans-
Introduction
- The pancreas is a soft, finely lobulated, elongated exo-endocrine gland.
- The exocrine part secretes the pancreatic juice and the endocrine part secretes the hormones, viz.,insulin, etc.
- The pancreas (in Greek pan: all, kreas: flesh).
- Pancreas named because of its fleshy appearance.
- The pancreatic juice helps in the digestion of lipids, carbohydrates, and proteins, whereas the pancreatic hormones maintain glucose homeostasis.
Location
- The pancreas lies more or less horizontally on the posterior abdominal wall.
- In the epigastric and left hypochondriac regions.
- It crosses the posterior abdominal wall obliquely from concavity of the duodenum to the hilum of spleen opposite the level of T12– L3 vertebrae.
- The greater part of the gland is retroperitoneal behind the serous floor of the lesser sac.
Size and Shape
- The pancreas is “J”-shaped or retort shaped being set obliquely.
- The bowl of retort represents its head and the stem of retort represents its neck, body, and tail.
Its measurements are-
- Length: 12–15 cm.
- Width: 3–4 cm.
- Thickness: 1.5–2 cm.
- Weight: 80–90 g.
Parts and Relations
For descriptive purposes, the pancreas is subdivided into four parts
- Head (with one process— uncinate process).
- Neck.
- Body (with one process—tuber omentale).
- Tail.
1. Head of the Pancreas and its relationship
- It is the enlarged, disc-shaped right end of the pancreas.
- lies in the concavity of the C-shaped duodenal loop in front of the L2 vertebra.
External Features
- The head presents the following external features
- Three borders- Superior, inferior, and right lateral.
- Two surfaces- Anterior and posterior.
- One process- Uncinate process. (It is a hook-like process from the lower and left part of the head.
Superior border is related to-
- First part of the duodenum.
- Superior pancreaticoduodenal artery.
Inferior border is related to-
- Third part of the duodenum.
- Inferior pancreaticoduodenal artery.
Right lateral border is related to-
- Second part of the duodenum, and anterior and posterior pancreaticoduodenal arterial arcades.
Anterior surface is related from above downward to
- Gastroduodenal artery,
- Transverse colon,
- Root of the transverse mesocolon,
- jejunum.
Posterior surface is related to-
- IVC.
- left renal vein,
- Bile duct (lying in a groove, and may be found embedded in the pancreatic tissue).
- Right crus of diaphragm.
Uncinate process is related to-
- Anteriorly to superior mesenteric vessels.
- Posteriorly to the abdominal aorta.
2. Neck of the Pancreas -
- It is a slightly constricted part of the gland which connects the head with the body.
- It is about 2.5 cm (1 inch) long and is directed forward, upward, and to the left.
External Features-
- Two surfaces- Anterior and posterior.
- Two borders- Upper and lower.
3. Body of the Pancreas
- It is the elongated part of the gland extending from its neck to the tail.
- It passes toward the left of midline with a slight upward and backward inclination.
- It lies in front of the vertebral column at or just below the transpyloric plane.
External Features
- It is somewhat triangular in cross section and presents
- Three borders: Anterior, superior, and inferior.
- Three surfaces: Anterior, posterior, and inferior.
- One process: Tuber omentale (a part of the body projects above the lesser curvature of the stomach and comes in contact with the lesser omentum across the lesser sac).
- Anterior border provides the attachment to the root of transverse mesocolon.
- Superior border is related to the coeliac artery above the tuber omentale, hepatic artery to the right, and splenic artery to the left of tuber omentale.
- Inferior border is related to superior mesenteric vessels (at its right end).
4. Tail of the Pancreas-
- It is the narrow left extremity of the pancreas.
- It lies in the lienorenal ligament along with splenic vessels.
- It is mobile unlike the other major retroperitoneal parts of the gland.
- It contains the largest number of islets of Langerhans per unit of tissue as compared to other parts of the gland.
Ducts of the Pancreas
Usually there are two ducts: main and accessory, which drain the exocrine secretion into the duodenum.
A. Main Pancreatic Duct-
- It begins in the tail and traverses the whole length of the gland near its posterior surface. At the neck, it turns downward, and then to the right to enter into the second part of duodenum.
- It joins the bile duct as it pierces the duodenal wall to form the hepatopancreatic ampulla (of Vater) which opens by a narrow mouth on the summit of major duodenal papilla 8–10 cm distal to the pylorus.
- It receives tributaries (smaller ducts) throughout its length, at right angle to its long axis in a “herringbone pattern.”
B. Accessory Pancreatic Duct
- It begins in the lower part of the head, and then runs upward and medially, crossing in front of main pancreatic duct.
- It opens into the second part of the duodenum on the summit of minor duodenal papilla about 2–3 cm above the opening of main pancreatic duct (6–8 cm distal to pylorus).
Arterial supply of the Pancreas
- Splenic artery, a branch of coeliac trunk
- Superior pancreaticoduodenal artery- The superior pancreaticoduodenal artery is a branch of gastroduodenal artery.
- Inferior pancreaticoduodenal artery- The inferior pancreaticoduodenal artery is a branch of superior mesenteric artery.
Venous Drainage
- Portal vein.
- Superior mesenteric vein,
- Splenic vein.
Lymphatic Drainage
- Pancreaticosplenic nodes (main group).
- Coeliac nodes.
- Superior mesenteric nodes.
- Pyloric nodes.
Nerve Supply
- The sympathetic and parasympathetic nerve fibres reach the gland along its arteries from coeliac and superior mesenteric plexuses
- The sympathetic supply is vasomotor whereas the parasympathetic supply controls the pancreatic secretion.
Q.2 Classification of joints with example
- Joint is a junction between two or more bones or cartilages. It is a device to permit movement.
- Joint are classified into structural and functional.
- Structural classification is determined by how the bones connect to each other, while functional classification is determined by the degree of movement between the articulating bones.
1. Structural classification
A. Fibrous(Fixed)
B. Cartilaginous(Slightly movable)
C. Synovial freely(Movable)
A. Fibrous(Fixed)-Fibrous/Immovable Fibrous/Immovable bones are connected by dense connective tissue, consisting mainly of collagen. The fibrous joints are further divided into three types
a. Sutures or synostoses are found between bones of the skull. In fetal skulls the sutures are wide to allow slight movement during birth.
b. Syndesmosis are found between long bones of the body, such as the radius and ulna in forearm and the fibula and tibia in leg. Unlike other fibrous joints, syndesmoses are moveable (amphiarthrodial), but not to such degree as synovial joints.
3. Gomphosis is a joint between the root of a tooth and the sockets in the maxilla or mandible.
B. Cartilaginous(Slightly movable)- Cartilaginous joints are connected entirely by cartilage. Cartilaginous joints allow more movement between bones than a fibrous joint but less than the highly mobile synovial joint. An example would be the joint between the manubrium and the sternum. Cartilaginous joints also form the growth regions of immature long bones and the intervertebral discs of the spinal column.
a. Primary cartilaginous joints - Known as "synchondroses". Bones are connected by hyaline cartilage or fibrocartilage, sometimes occurring between ossification centers. This cartilage may ossify with age. These joints usually allow no movement, or minimal movement in the case of the manubriosternal and first manubriocostal joints.
- Examples in humans are the joint between the first rib and the manubrium of the sternum, and the "growth plates" between ossification centers in long bones.
b. Secondary cartilaginous joints - Known as "symphyses". Fibrocartilaginous joints, usually occurring in the midline. Examples in human anatomy would be the intervertebral discs, and the pubic symphysis. Articulating bones at a symphasis are covered with hyaline cartilage and have a thick, fairly compressable pad of fibrocartilage between them.
C. Synovial Freely(Movable)-
- Articular ends covered in hyaline cartilage and held together by dense connective tissue
- Joint capsules made up of ligaments (outer layer) and synovial membranes (inner layer)
There are six types of synovial joints
- Ball and Socket - such as the shoulder or the hip and femur.
- Hinge - such as the elbow.
- Pivot - such as the radius and ulna.
- Condyloid (or ellipsoidal) - such as the wrist between radius and carpals, or knee
- Saddle - such as the joint between carpal thumbs and metacarpals.
- Gliding - such as between the carpals.
2. Functional Classification
- Synarthrosis - Synarthroses permit little or no mobility. Most synarthrosis joints are fibrous joints.Egcranial sutures in adult.
- Amphiarthrosis -Amphiarthroses permit slight mobility. The two bone surfaces at the joint are both covered in hyaline cartilage and joined by strands of fibrocartilage. eg: secondary cartilaginous joints
- Diarthrosis- Permit a variety of movements. Only synovial joints are diarthrodial.
3. Classification According to number of articulating bones
- Simple Joint- 2 articulation surfaces (eg. shoulder joint, hip joint)
- Compound Joint- 3 or more articulation surfaces (eg. radiocarpal joint)
- Complex Joint- 3 or more articulation surfaces and an articular disc or meniscus (eg . knee joint)
Q.3 Muscles of upper limb
Muscles of Upper Limb
- The upper limb is a multi jointed lever that is freely movable on the trunk at the shoulder joint. At the distal end of the upper limb is important organ.
- The upper limb is divided in to the shoulder (junction of the trunk with the arm) arm, elbow, forearm, wrist and hand.
Muscles of shoulder and arm region
1. Pectoralis Major
| Oring | Insertion | Innervation | Action |
|
Sternal end of clavicle, sternum, cartilage of ribs 1-6, & aponeurosis of external oblique muscle |
By a short tendon into intertubercular groove of humerus | Lateral & medial pectoral nerves |
|
2. Pectoralis Minor
| Oring | Insertion | Innervation | Action |
| Anterior surface of ribs 3-5 (or 2-4) | Coracoid process of scapula | Both pectoral nerves |
|
3. Serratus Anterior
| Oring | Insertion | Innervation | Action |
| By series of muscle slips from ribs 1-9 | Anterior surface of vertebral border of scapula | Long thoracic nerve |
|
4. Subclavius
| Oring | Insertion | Innervation | Action |
| Costal cartilage of rib 1 | Groove on inferior surface of clavicle | Nerve to subclavius | Stablizes & depresses pectoral girdle |
5. Trapezius
| Oring | Insertion | Innervation | Action |
|
Occipital bone, ligamentum nuchae, spines of C7 - T12 |
Spine & acromion of scapula, lateral 3rd of clavicle | Accesory nerve |
|
6. Levator scapulae
| Oring | Insertion | Innervation | Action |
| Transverse processes of C1-C4 | Medial border of scapula, superior to spine | Cervical spinal nerves & dorsal scapular nerve |
|
6. Rhomboid minor and major
| Oring | Insertion | Innervation | Action |
|
|
Medial border of scapula |
|
| Rhomboid major | Spinous processes of T2- T5 | Medial border of scapula |
7. Latissimus dorsi
| Oring | Insertion | Innervation | Action |
| Via lumbodorsal fascia into spines of T7-L5, lower 4 ribs & iliac crest | Floor of intertubercular groove of humerus | Thoracodorsal |
|
8. Deltoid
| Oring | Insertion | Innervation | Action |
| Lateral 3rd of clavicle, acromion & spine of scapula | Deltoid tuberosity of humerus | Axillary nerve |
|
9. Supraspinatus
| Oring | Insertion | Innervation | Action |
| Supraspinous fossa of scapula | Superior part of greater tubercle of humerus | Suprascapular nerve |
|
9. Infraspinatus
| Oring | Insertion | Innervation | Action |
| Infraspinous fossa of scapula | Greater tubercle of humerus, posterior to supraspinatus | Suprascapular nerve |
|
10. Teres minor
| Oring | Insertion | Innervation | Action |
| Lateral border of dorsal scapular surface | Greater tubercle of humerus, inferior to infraspinatus | Axillary nerve | Same as infraspinatus |
11. Teres major
| Oring | Insertion | Innervation | Action |
| posterior surface of scapula; inferior angle | Intertubercular groove of humerus, tendon fused with tendon of latissimus dorsi | Lower scapular nerve |
|
12. Subscapularis
| Oring | Insertion | Innervation | Action |
| Subscapular fossa of scapula | lesser tubercle of humerus | Subcapular nerve |
|
13. Coracobrachialis
| Oring | Insertion | Innervation | Action |
| Coracoid process of scapula | Medial surface of humerus shaft | Musculocutaneous nerve |
|
14. Rotator Cuff Muscles
Consists 4 muscles
- S – Supraspinatus
- I – Infraspinatus
- T – teres minor
- S – Subscapularis
Group of muscles that stabilize GH joint.
B. Muscles of forearm
Muscles that act on the forearm
1. Triceps brachii
a. Action – Extend forearm
b. Origin
- Long head-infraglenoid tubercle of the scapula
- Lateral Head-posterior surface above radial groove.
- Middle Head-posterior humerous below radial groove.
c. Insertion– Olecranon process of the Ulna
THE 3 B’S THAT BEND THE ELBOW-
- Biceps brachii
- Brachioradialis
- Brachialis
Pronators and Supinator Pronators
Pronator Quadratus
- Action-Pronates the hand
- Origin- the distal 4th of the ulna
- Insertion- distal 4th of the radius
Pronator Teres
- Action-Pronates forearm
- Origin- the medial epicondyle of the humerus and coronoid process of the ulna
- Insertion- Lateral surface of the radius.
C. MUSCLES THAT MOVE WRIST, HAND AND DIGITS
1. Palmar Interosseous muscles
- Action – Adduct digits 2,4 and 5
- Origin – palmar surface of metacarpals 2,4,5
- Insertion: – sides of proximal phalange bases for fingers 2,4,5
2. Dorsal Interosseous Muscles
- Action – Abduct digits 2-4
- Origin – adjacent sides of metacarpal bones.
- Insertion: – dorsal tendons on fingers 2-5
3. Thenar Group
Flexor pollicis brevis Opponens pollicis Abductor pollicis brevis
Actions-
- Flexes thumb
- Abducts thumb
- Opposition of thumb
4. Hypothenar Group
Flexor digiti minimi brevis Abductor digiti minimi Opponens digiti minimi
Actions
- Flexes finger 5
- Abducts pinky
- Opposition of pinky
Q.4 Blood supply of kidney
Introduction
- The kidneys are bilateral, bean shaped organs that are situated retroperitoneally. The organs lie along the posterior abdominal wall, where they filter blood, maintain ionic homeostasis and produce urine. The body of the liver displaces the right kidney inferiorly, resulting in the left kidney being slightly superior to the right.
- Along the medial surface, there is a concavity known as the hilum. At this point, the renal arteries enter, and the renal veins and pelvis (beginning of the ureters) leave the kidney.
- The neural supply from both divisions from the autonomic nervous system also enters the kidney at the hilum.
- Lymphatic drainage from both the renal cortex (outer layer of kidney) and renal medulla (inner layer of kidney) go to the same group of nodes.
Arterial supply
- The abdominal aorta gives off many branches, including the renal arteries. The renal arteries branch off perpendicular to the abdominal aorta, travelling posterior to the renal veins, nerves and the pancreas.
- Subsequent to branching from the aorta, the renal artery enters the kidney at the hilum, where it divides into anterior and posterior branches. The posterior division goes on to supply the posterior region of the kidney, while the anterior branch divides further to produce apical, anterior superior, anterior inferior and inferior segmental arteries; each supplying their respective segments.
- At the level of the minor calices, the branches of the anterior renal arteries further divides into interlobar arteries that course around the borders of the medullary pyramids. At the base of the pyramids, these arteries are referred to as arcuate arteries.
- Finally, the arteries enter the nephrons (functional units of the kidneys) as the interlobular arteries, where afferent arterioles bring blood to the glomerulus to be filtered. It should be noted that these arteries neither anastomose nor have accompanying veins.

Capillary network
- As the afferent arterioles enter the glomerulus, they form an intricate network of communicating capillaries. The capillaries are lined by a unique fenestrated epithelium (each space being around 70 – 100 nm wide). The fenestration allows selective passage of smaller particles into the renal tubules and keeps larger blood cells in the vessels.
- The capillaries leave the glomerulus as efferent arterioles, after which they form capillary beds around the nephron’s loop of Henle. In cortical nephrons (loop of Henle does not extend deep into the medulla), the capillary beds are called peritubular capillaries; while in juxtamedullary nephrons (loop of Henle extends deep into the medulla), the capillary beds are called vasa recta. These capillary beds facilitate blood pressure regulation and ionic homeostasis both passively and under hormonal influence.
Venous drainage
- As the capillaries leave the nephron, they condense to form interlobular veins. Similar to the branches of the renal arteries, the interlobular veins become arcuate veins at the base of the medullary pyramids, then interlobar veins. About five or six interlobar veins join together to form each renal vein. Unlike the branches of the renal arteries, the tributaries of the renal vein communicate with each other.
Lymphatic drainage
- Superficial lymphatic vessels form a plexus under the renal capsule (thin layer covering the kidneys) known as the subcapsular lymphatic plexus. They, along with medullary lymph vessels, communicate with cortical lymph vessels that travel alongside interlobular, arcuate and interlobar arteries. The renal lymphatics then drain directly to the lumbar lymph trunks (which then drain to the thoracic duct and cisterna chyli) and to para-aortic nodes, including precaval, lumbar and postcaval nodes.
3. Very short questions (Attempt any three): 3x2=6
- Structure of neuron
Neuron Definition
“Neurons are the fundamental unit of the nervous system specialized to transmit information to different parts of the body.”
What is a Neuron
Neurons are the building blocks of the nervous system. They receive and transmit signals to different parts of the body. This is carried out in both physical and electrical forms. There are several different types of neurons that facilitate the transmission of information.
Neuron Structure
A neuron varies in shape and size depending on its function and location.
-
Cell Body
-
Axons
-
Dendrites
-
Neurilemma
-
Myelin Sheath
-
Node of Ranvier
-
Synapse

Cell Body
-
Part of neuron containing nucleus but not incorporating axon and dendrites.
Axons
-
Long, slender projection of a nerve cell
-
Conducts electrical impulses away from neuron’s cell body
-
Function - Transmit information to different neurons, muscles and glands
Dendrites
-
Branched projections of a neuron.
-
Conduct the electro chemical stimulation received from other neural cell to the cell body of the neuron from which the dendrites project.
Neurilemma
-
Outermost nucleated cytoplasmic layer
-
Surrounds axon of the neuron.
-
Forms the outermost layer of the nerve fibre in the Peripheral Nervous System.
Myelin Sheath
-
Fatty material made by glial cells
-
Insulates the axon
-
Allows rapid movement of electrical impulses along axon.
Node of Ranvier
-
Gaps in myelin sheath where action potential are terminated
-
Multiple sclerosis is a breakdown of nodes of ranvier.
Synapse
-
Junction where the axon or some other portion of one cell terminates on the dendrites, soma or axon of another neuron.
Q.2 Clinical significance of prostate gland
Ans
Prostate gland-
- The prostate gland is the accessory reproductive structure in males.
- It lies around the urethra at the base of the neck region of the urinary bladder and is covered by a vascular capsule.
Functions-
- Prostate gland secretes prostatic fluid
- This prostatic fluid is thin, milky and slightly acidic and it forms 30% of the seminal fluid.
- It helps in the movement of sperm.
Q.3 Layers of uterus
The uterus has three layers
1. Perimetrium The outer layer of tissue made of epithelial cells. It is the protective layer.
2. Myometrium- The middle layer made of smooth muscle tissue. It expands during pregnancy and contracts to push the baby out.
3. Endometrium- The inner layer or lining of the uterus. It is lined with simple columnar epithelium and contains tubular glands. It is shed during the menstrual cycle or the period.
subdivided into 2 parts-
- Deep stratum basalis- Changes little throughout the menstrual cycle and is not shed at menstruation.
- Superficial stratum functionalis- Proliferates in response to oestrogens, and becomes secretory in response to progesterone. It is shed during menstruation and regenerates from cells in the stratum basalis layer.
Q.4 Labes of lungs
Lobes and Fissures
A. Right Lung
The right lung is slightly larger than the left and id divided by the oblique and horizontal fissures in to three lobes-
- The upper lobe
- Middle lobe
- Upper lobe
- The oblique fissure runs from the inferior border upwards and backward across the medial and costal surfaces, crossing the posterior border about 6 cm below the apex and inferior border about 5 cm from the medial plane.
- The horizontal fissure runs horizontally across the costal surface at the level of the 4th costal cartilage to meet the oblique fissure in the midaxillary line. The middle lobe is thus a small triangular lobe bounded by the horizontal and oblique fissures.

B. Left Lung
The left lung is divided by an oblique fissure into two lobes, the upper and lower lobes . There is no horizontal fissure in the left lung.
Section-B (Applied Physiology)
1. Long/Essay type questions (Attempt any one): 1x10=10
- Explain mechanism of respiration in detail.
Respiration - The series of exchanges that leads to the uptake of oxygen by the
cells, and the release of carbon dioxide to the lungs
Mechanics Of Respiration-
- Mechanism of respiration involves the breathing mechanism and exchange of gases. The gaseous exchange occurs by diffusion in the alveoli. It depends upon the pressure differences between blood and tissues, or atmospheric air and blood. The exchange of gases takes place at the surface of the alveolus.
Mechanism Of Breathing
The air which we breathe in and out of the lungs varies in its pressure. So basically when there is a fall in air pressure the alveolar spaces falls and the air enters the lungs (inspiration) and as the pressure of the alveoli within exceeds the atmospheric pressure, the air is blown from the lungs (expiration). The flow rate of air is in proportion to the magnitude of the pressure difference.
The breathing mechanism involves two processes-
- Inspiration.
- Expiration.
1. Inspiration
- The process of intake of atmospheric air is known as inspiration. It is an active process.
- In the process of inspiration, there would be a contraction of muscles attached to the ribs on the outer side which pulls out the ribs and results in the expansion of the chest cavity.
- Later, the diaphragm, contracts, moves downwards and expands the chest cavity resulting in the contraction of the abdominal muscles.
- The expansion of the chest cavity produces a partial vacuum which sucks air into the lungs and fills the expanded alveoli.

Mechanism of Inspiration
- When the volume of the thoracic cavity increases and the air pressure decreases, inspiration takes place.
- Contraction of external intercostal muscles increases the volume of the thoracic cavity.
- Contraction of the diaphragm further increases the size of the thoracic activity. Simultaneously, the lungs expand.
- With the expansion of the lungs, the air pressure inside the lungs decreases.
- The pressure equalizes and the atmospheric air rushes inside the lungs.
B. Expiration
- The process of exhaling carbon dioxide is called expiration. It is a passive process.
- The expiration process is considered once after the gaseous exchange occurs in the lungs and the air is expelled out.
- During this process, muscles attached to the ribs contract, the muscles of the diaphragm and the abdomen relax which leads to a decrease in the volume of the chest cavity and increases the pressure of the lungs, causing the air in the lungs to be pushed out through the nose.

Mechanism of Expiration
- It occurs when the size of the thoracic activity decreases and the air pressure outside increases.
- Now the external intercostal muscles relax and the internal intercostal muscles contract.
- As a result, the ribs are pulled inwards and the size of the thoracic cavity is reduced.
- The diaphragm is relaxed and the lungs get compressed.
- Consequently, the pressure increases and the air is forced outside.
Exchange Of Gases
The gaseous exchange occurs by diffusion in the alveoli. It depends upon the pressure differences between blood and tissues, or atmospheric air and blood. The exchange of gases takes place at the surface of the alveolus.

The exchange of gases takes place in the following manner-
- Transport Of Oxygen.
- Internal Respiration.
- Transport Of Carbon dioxide From Tissues To Lungs.
- Intrapleural Breathing.
- Respiratory Gas Transport.
1. Transport Of Oxygen
Oxygen in the blood is carried to the tissue in two forms
- Oxyhaemoglobin Chemical composition of oxygen with haemoglobin, and solution of oxygen in the blood plasma. The oxygen in the blood combines with haemoglobin when the concentration of oxygen is high in the blood.
- Oxyhemoglobin being unstable, dissociates to release oxygen. Low oxygen, low pH and high temperatures stimulate the dissociation process.
2. Internal Respiration
- The gaseous exchange taking place in the tissues is called internal respiration. Here, the oxygen carried in the form of oxyhemoglobin gets dissociated to release oxygen.
- This oxygen breaks down the glucose to release carbon dioxide, water, and energy. The energy is utilized by the body, while the carbon dioxide is diffused from the tissues.
3. Transport Of Carbon dioxide From Tissues To Lungs
Carbon dioxide is transported by three mechanisms-
- Some carbon dioxide dissolves in the water of plasma to form carbonic acid. Carbonic acid ionizes to form bicarbonate ions. The hydrogen ions are catalyzed by the enzyme carbonic anhydrase. Bicarbonate ions combine with sodium and potassium to form sodium bicarbonate and potassium bicarbonate.
- Some carbon dioxide combines with haemoglobin for the formation of carbaminohemoglobin. It is finally carried to the lungs and released out of the body through expiration.
4. Intrapleural Breathing
- Intrapleural breathing is used to refer to the pressure that is present in the space between the pleura and the lungs. This space is referred to as the pleural cavity. The pressure in this region is normally less than the atmospheric pressure. Pleural pressure is termed as negative pressure.
- The lung movement is governed by the pressure gradient, the transpulmonary pressure, which exists between the pleura and the lungs. The difference in the pressures between the intrapulmonary and intrapleural pressures is known as transpulmonary pressure.
- The pressure in the pleural cavity while breathing turns negative while there is an increase in the transpulmonary pressure causing the lungs to expand. While expiration, the lungs recoil as a result of an increase in the pleural pressure.
- The competing forces inside the thorax results in the formation of the negative intrapleural pressure, one of these forces is associated with the lungs elasticity. The lungs have elastic tissues which cause it to be pulled inwards off the thoracic wall. An inward pull of the lung tissue is also generated by the surface tension of the alveolar fluid. The inward tension generated from the lungs is opposed by forces from the thoracic wall and the pleural fluid.
5. Respiratory Gas Transport
- After the gases have scattered in the lungs, causing the blood to become oxygenated, leaving carbon dioxide, the next phase of transportation of oxygen-rich blood to the tissues takes place. Meanwhile, the next round of deoxygenated blood needs to be brought to the lungs for the cycle to continue.
- In the bloodstream, the transportation of gases occurs all through the body which is contributed to the cardiovascular system comprising of the blood vessels and the heart. The blood carrying oxygen leaves the lungs to flow into the heart through the pulmonary veins, which are pumped to the rest of the body from the left ventricle through the aorta and its corresponding branches.
Q. 2 Describe name, functions and diseases caused by alteration of adrenal gland hormones.
Adrenal Gland
The Adrenal Glands are found on top of each kidney. Even the name “Adrenal” directly refers to their location: (Latin: ad– “near” and renes – “kidneys.”) These glands are also known as suprarenal glands. (Latin: supra – “above” and renes – “kidneys.”)
Adrenal Gland Hormones
Adrenal Cortex-The adrenal cortex is red to light brown in colour and is composed of three zones. The adrenal cortex represents 80-90% of the adrenal gland. The adrenal medulla represents only 10-20% of the adrenal gland.
A. Hormones of the Adrenal Cortex
The adrenocortical hormones and their functions in the body are classified into
- Mineralocorticoids
- Glucocorticoids
- Adrenal androgens

1. Mineralocorticoids-These hormones help to control the water and electrolyte homeostasis, particularly the concentration of Na+ and K+ ions. Mineralocorticoids include the following hormones:
- They are produced in the zona glomerulosa.
- The primary mineralocorticoid is aldosterone. Its secretion is regulated by the oligopeptide angiotensin II (angiotensin II is regulated by angiotensin I, which in turn is regulated by renin).
- Aldosterone is secreted in response to high extracellular potassium levels, low extracellular sodium levels, and low fluid levels and blood volume.
Aldosterone affects metabolism in different ways-
- It increases urinary excretion of potassium ions.
- It increases interstitial levels of sodium ions.
- It increases water retention and blood volume.
2. Glucocorticoids
- They are produced in the zona fasciculata.
- The primary glucocorticoid released by the adrenal gland in the human is cortisol and corticosterone in many other animals.
- Its secretion is regulated by the hormone ACTH from the anterior pituitary.
Upon binding to its target, cortisol enhances metabolism in several ways-
- It stimulates the release of amino acids from the body
- It stimulates lipolysis, the breakdown of fat
- It stimulates gluconeogenesis, the production of glucose from newly-released amino acids and lipids
- It increases blood glucose levels in response to stress, by inhibiting glucose uptake into muscle and fat cells
- It strengthens cardiac muscle contractions
- It increases water retention
- It has anti-inflammatory and anti-allergic effects
3. Androgens
Androgen, also called androgenic hormones or testoids, is the generic term for any natural or synthetic compound, usually a steroid hormone, that stimulates or controls the development and maintenance of male characteristics in vertebrates by binding to androgen receptors.
- This includes the activity of the accessory male sex organs and development of male secondary sex characteristics.
- Androgens were first discovered in 1936.
- Androgens are also the original anaboli steroids and the precursor of all estrogens, the female sex hormones.
- The primary and most well-known androgen is testosterone.
- Androgen ablation can be used as an effective therapy in prostate cancer.
B. Adrenal medulla
- The adrenal medulla is part of the adrenal gland.
- It is located at the center of the gland, being surrounded by the adrenal cortex.
- It is the inner most part of the adrenal gland, consisting of cells that secrete epinephrine, norepinephrine, and a small amount of dopamine in response to stimulation by sympathetic preganglionic neurons.
a. Epinephrine (Also called adrenaline)
- Epinephrine (also known as adrenaline) is a hormone and neurotransmitter.
- It increases heart rate, contracts blood vessels, dilates air passages and participates in the fight-or- flight response of the sympathetic nervous system.Chemically, epinephrine is a catecholamine, a monoamine produced only by the adrenal glands from the amino acids phenylalanine and tyrosine.
- The term adrenaline is derived from the Latin roots ad- and renes and literally means on the kidney, in reference to the adrenal gland's anatomic location on the kidney.
b. Norepinephrine (Also called noradrenaline.)
- Norepinephrine (INN) (abbreviated norepi or NE) or noradrenaline (BAN) (abbreviated NA or NAd) is a catecholamine with multiple roles including as a hormone and a neurotransmitter.
- As a stress hormone, norepinephrine affects parts of the brain where attention and responding actions are controlled.
FUNCTIONS
Function of adrenal medulla
- Rather than releasing a neurotransmitter, the cells of the adrenal medulla secrete hormones.
- Notable effects of adrenaline and noradrenaline include increased heart rate and blood pressure, blood vessel constriction in the skin and gastrointestinal tract, blood vessel dilation in skeletal muscles all of which are characteristic of the fight-or-flight response. Release of catecholamines is stimulated by nerve impulses, and receptors for catecholamines are widely distributed throughout the body.
Functions of adrenal cortex-
- It stimulates the release of amino acids from the body.
- It stimulates lipolysis, the breakdown of fat.
- It increases urinary excretion of potassium ions.
- It increases interstitial levels of sodium ions.
- It increases water retention and blood volume.
- Testes formation
- Spermatogenesis
Adrenal Gland Disorders
Adrenal Gland disorders appear when not enough hormones or inadequate hormones are produced by the adrenal glands. Even abnormal growths or tumours can cause certain illness.
- Cushing’s Syndrome is a condition where the cortisol levels in the body are very high. The cause can be a tumour in the adrenal gland or the pituitary gland.
- Adrenocortical carcinoma is a cancerous tumour that usually develops in the outer layer of the adrenal gland. This type of tumour is typically found years after they have spread to other organs in the body.
- Congenital Adrenal Hyperplasia (CAH) is a genetic disorder characterized by very low levels of cortisol production. The people inflicted with this condition may also have other hormonal imbalances where their bodies may make very little aldosterone, but too much androgen.
- Addison’s Disease is caused when adrenal glands produce insufficient cortisol or aldosterone. It results in weakness, fatigue, low blood pressure, nausea, etc. In 70% of cases, Addisone disease is caused due to autoimmune disorder, where the body mistakenly attacks the adrenal glands. As a result, the adrenal gland does not produce the hormone aldosterone in sufficient quantities.
2. Short notes (Attempt any three): 3x5=15
- Explain cardiac cycle
Cardiac cycle-
Cardiac cycle is defined as the succession of (sequence of) coordinated events taking place in the heart during each beat. Each heartbeat consists of two major periods called systole and diastole.
- During systole, heart contracts and pumps the blood through arteries.
- During diastole, heart relaxes and blood is filled in the heart.
Events of cardiac cycle are classified into two
- Atrial events
- Ventricular events.

Duration of cardiac Cycle-
When the heart beats at a normal rate of 72/minute, duration of each cardiac cycle is about 0.8 second.
Atrial events are divided into two divisions-
a. Atrial systole
- Atrial systole = 0.11 (0.1) sec
- Coincide with last rapid filling phase of ventricles.
- Before this valves are open, ventricles relaxed with already 75% blood
- Contraction add only remaining 25% blood.
2. Atrial diastole
- Atrial diastole = 0.69 (0.7) sec
- Coincide with Ventricular Systole & most of the ventricular diastole.
- Atria Relax – gradual filling of atria – pressure slowly increases.
Ventricular events are divided into two divisions-
a. Ventricular systole
- Ventricular systole = 0.27 (0.3) sec
- Phase of Iso-Volumic (Iso-metric) Contraction
- Phase of ventricular ejection.
- Rapid phase
- Slow phase.
- Phase of Iso-Volumic (Iso-metric) Contraction (0.05)
- When intra-ventricular pressure rises closes AV valves semilunar valves not yet open so contracts as closed chamber.
- No change in volume so called Iso-Volumic contraction.
- Sharp rise in Intraventricular pressure.
- Phase of ventricular ejection (0.25) begins with opening of semilunar valves.
- Rapid phase (0.1) – 2/3rd of stroke volume ejected.
- Slow phase.(0.15) – 1/3rd of stroke volume ejected.
b. Ventricular diastole
- Ventricular diastole = 0.53 (0.5) sec.
- Protodiastole
- Isovolumic or Isometric Relaxation phase.
- Rapid passive filling phase.
- Reduced filling & Diastosis
- Last rapid filling phase.
Q.2 Composition and functions of saliva
Saliva
According to Stedmen's Dictionary
- Saliva is a clear, tasteless, odourless slightly acidic (pH6.8), viscid fluid, consisting of secretions from the parotid, sublingual and submandibular salivary gland and the mucous glands of the oral cavity.
According to Webster Medical Dictionary
- The watery tasteless liquid mixture of salivary & oral mucous glands secretion that lubricates the chewing food , wets the oral wall & contains the enzyme ptyalin which function in the pre-digestion of starch.
Composition of Salvia
The parotid gland secretion is a watery secretion containing enzyme amylase, while lingual and sub mandibular secretion is viscous and contain mucous. This is due to the presence of serous cells in parotid gland and mainly mucous secreting cells in the lingual and sub mandibular gland.
Saliva contains 99% of Water and 1% solids. Solids substances are both organic and inorganic components: Organic substances include enzymes, like alpha-amylase (ptyalin), lingual lipase, kallikrein, lysozyme, small amounts of urea, uric acid, cholesterol and mucin. Inorganic substances are sodium (Na+), Chloride (Cl-), Potassium (K+) and bicarbonate (HCO3-)

Function of Salvia
Saliva is very essential . Since it has many functions , its absence leads to many inconveniences.
- Preparation of food for swallowing- When food enters the mouth , saliva moistens and dissolves it. The mucous membrane of mouth is also moistened and masticated food is rolled into a bolus. The mucin of saliva lubricates the bolus and facilitates the swallowing
- Appreciation of taste-Taste is a chemical sensation. Saliva by its solvent action dissolves the solid food substance , so that the dissolved substances can stimulate the taste buds.The stimulated taste buds recognize the taste.
- Digestive function- Saliva has three digestive enzymes namely,salivary amylase,maltase,and lingual lipase.salivary amylase is a carbohydrate splitting(amylolytic)enzyme. The enzyme maltase is present only in traces in human saliva. • It converts maltose into glucose.The lingual lipase is secreted from serous glands situated on the posterior aspect of tongue
- Cleansing and protective functions- Due to the constant secretion of saliva,the mouth and teeth are rinsed and kept free from food debris,shed epithelial cells and foreign particles. In this way,saliva prevents bacterial growth by removing materials,which may serve as culture media for the bacterial growth. the enzyme lysozyme of saliva kills some bacteria such as staphylococcus,streptococcus,and brucella. mucin present in the saliva protects the mouth by lubricating the mucous membrane of the mouth.
- Role in speech- By moistening and lubricating the soft parts of mouth and lips,saliva helps in speech. If the mouth is dry,articulation and pronunciation become difficult.
- Excretory function- Many substances,both organic and inorganic,are excreted in saliva. It excretes substances like mercury,potassium iodide,lead and thiocyanate. Saliva also excretes some viruses such as those causing rabies and mumps In some pathological conditions, saliva exretes substances like sugar in diabetes mellitus, calcium in hyperparathyroidism.
- Regulation of body temperature-In dogs and cattle excessive dripping of saliva during panting helps in loss of heat and regulation of body temperature. However,in human being sweat glands play major role in the temperature regulation and saliva does not play any role in this function.
- Regulation of water balance-When the body water content decreases ,salivary secretion also decreases. This causes dryness of the mouth and induces thirst. When the water is taken,it quenches the thirst and restores the body water content.
Q.3 Blood group types
- Dr. Karl Landsteiner's discovered the ABO Blood Group System in 1901.
- He and five co-workers began mixing each others red blood cells and serum together and accidentally performed the first forward and reverse ABO groupings.
- Blood group, also known as blood type, is a category (type) of blood groups based on the presence and absence of blood group antigens in the surface (membrane) of the RBCs, and antibodies on the plasma.
Antigen
- An antigen is a substance usually a protein which when introduced into an individual who recognizes it as foreign, leads to the production of antibody. This antibody specifically reacts with the antigen. On the red cell surface there is presence of glycoproteins and glycolipids which act as antigens. They are called blood group antigens. These antigens can be on the surface, below or protrude from the red cell membrane. If introduced into the body of an individual who lacks the antigen, an immune reaction can occur.
Antibodies
- These are immunoglobulins present in the serum and can be of 5 types: IgG, IgM, IgD, IgA and IgE.
- If red cells carrying an antigen are introduced into the circulation of an individual who lacks that antigen, antibodies will form and cause destruction of the introduced red cells.
- These are immune or acquired antibodies and are IgG in nature.
- They react best at 37°C.Certain antibodies occur without antigenic stimulus and are called naturally occurring antibodies e.g. ABO antibodies. They are IgM in nature and reactat room temperature.
The ABO grouping system
The ABO grouping system is subdivided into 4 types based on the presence or absence of antigens A and B on the red cell surface as shown below.
- Red cells that only have antigen A are called group A.
- Those that only have B antigen are called group B.
- Cells that have both A and B antigens are group AB.
- Cells that lack both antigens are O
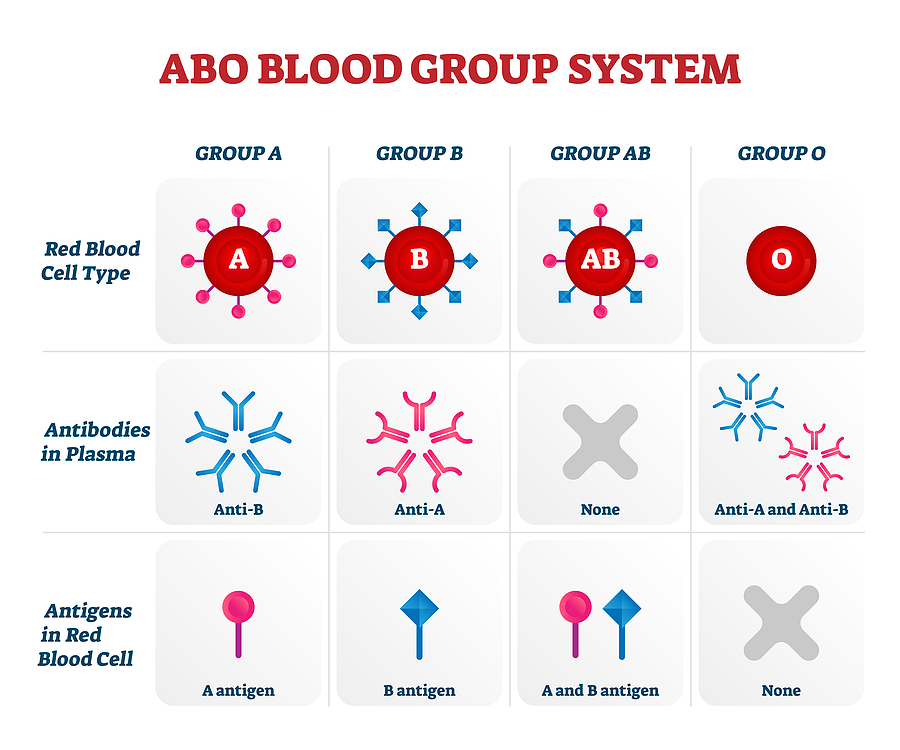
- Blood having antigen A belongs to A group. This blood has B antibody in the serum.
- Blood with antigen B and a antibody belongs to B group.
- If both the antigens are present, blood group is called AB group and serum of this group does not contain any antibody.
- If both the antigens are absent, blood group is called O group and serum of this group contain any a & b antibodies are present in the serum.
- Thus, RBC of "O" group has no antigen and so agglutination does not occur with any other group of blood. So,"O" group blood can be given to any blood group persons and the people with this blood group are called universal donors
- Plasma of AB group blood has no antibody. This does not cause agglutination of RBC from any other group of blood. People with AB group can receive blood from any blood group persons. So, people with this blood group are called universal recipients.
Q.4 Functions of skin
Functions of the Skin -The human skin is the outer covering of the body and is the largest organ of the integumentary system.
A. Protection-
- Skin protects underlying tissue from mechanical, chemical, and thermal injury.
- Keratin waterproofs the cells, preventing fluid loss and gain through the skin.
- Skin provides the first line of defense against bacteria and other pathogens.
- Melanin absorbs UV light Protection.
B. Sensory Reception
- Dermis contains sense receptors for heat, cold, pain, touch, and pressure
- Receptors clustered around hair follicles can detect if the hair moves
C. Temperature Regulation
Skin regulates body temperature in 2 ways:
- Sweat glands
- Dilation and constriction of blood vessels in the dermis
E. Synthesis of Vitamin D
- Skin cells contain a precursor molecule that is converted to vitamin D when exposed to UV light
- Vitamin D is essential for bone mineralization.
- Limited sun exposure can lead to vitamin D deficiency, which can result in osteoporosis and other chronic disorders.
F. Absorption through the skin
- Oxygen, nitrogen and carbon dioxide can diffuse into the epidermis in small amounts
- Some animals use their skin as their sole respiration organ
- In humans, the cells comprising the outermost 0.25–0.40 mm of the skin are "almost exclusively supplied by external oxygen"
- Some medications are absorbed through the skin
G. Control of Evaporation
- The skin provides a relatively dry and semi- impermeable barrier to reduce fluid loss
H. Water resistance
- The skin acts as a water resistant barrier so essential nutrients aren't washed out of the body
I. Storage
- Acts as a storage center for lipids and water
J. Camouflage
- Whether the skin is naked or covered in fur, scales, or feathers, skin structures provide protective coloration and patterns that help to conceal (hide) animals from predators or prey
3. Very short questions (Attempt any three): 3x2=6
Q.1 Fertilization-
Fertilization Definition
Fertilization is the process by which male and female gametes are fused together, initiating the development of a new organism.
The male gamete or ’sperm’, and the female gamete, ’egg’ or ’ovum’ are specialized sex cells, which fuse together to begin the formation of a zygote during a process called sexual reproduction.
- “Fertilization in humans refers to the fusion of male and female gametes that facilitates the development of a new organism.”
- Fertilization is the natural life process, which is carried out by the fusion of both male and female gametes, which results in the formation of a zygote. In humans, the process of fertilization takes place in the fallopian tube.
- During this process, semen comprising thousands of sperms are inseminated into the female vagina during coitus. The sperms move towards the uterus and reach the opening of the fallopian tube. only a few sperms will succeed in reaching the opening of the fallopian tube.
- The secondary oocyte releases from the matured Grafian follicle of the ovary and enters into the fallopian tube, where it is fertilized within 24 hours, after which it is released from the ovary.
- Though surrounded by several sperms, the oocyte is fertilized by a single sperm. During meiosis-II, the sperm enters the secondary oocyte and completes the meiosis. After this, the secondary oocyte is known as the egg.
- Both sperm and egg can show their vitality only to a limited period. Sperm is alive for 48-72 hours in a female reproductive system, whereas the egg can be fertilized for 24 hours before it is released.
Q.2 Functions of hypothalamus
The hypothalamus, a small region deep within the brain, regulates many critical functions, including:
- Maintaining body temperature.
- Controlling hormone release.
- Regulating thirst and hunger.
- Impacts the individual's sleep habits.
- Plays a role in the expression of emotions.
- Affects the autonomic nervous system.
- Controls reproductive functions.
- Sets off stress responses by triggering the release of stress hormones. The hypothalamus links the neurological and endocrine (hormonal) systems, controlling vital biological functions that contribute to general balance and well-being.
Q.3 Nerve impulse conduction-
- Nerve impulse refers to the generation of action membrane potential beyond the cell membrane in response to the stimulus. “Nerve impulse conduction” refers to the propagation of nerve impulse that occurs due to a change in membrane potential beyond the cell membrane.
- A nerve impulse is the electric signals that pass along the dendrites to generate a nerve impulse or an action potential. An action potential is due to the movement of ions in and out of the cell. It specifically involves sodium and potassium ions. They are moved in and out of the cell through sodium and potassium channels and sodium-potassium pump.
- Conduction of nerve impulse occurs due to the presence of active and electronic potentials along the conductors. Transmission of signals internally between the cells is achieved through a synapse. Nerve conductors comprise relatively higher membrane resistance and low axial resistance. The electrical synapse has its application in escape reflexes, heart and in the retina of vertebrates. They are mainly used whenever there is a requirement of fast response and timing being crucial. The ionic currents pass through the two cell membrane when the action potential reaches the stage of such synapse.
Nerve Impulse Conduction
- Continuous and saltatory conduction are the two common modes that facilitate the propagation of nerve impulse.
Continuous Conduction
- It refers to the non-myelinated conduction, where the flow of nerve-impulse is slower (0.1 m/s). It occurs in unmyelinated axons, where the ions flow throughout the axon segment via voltage-gated channels.
Saltatory Conduction
- It refers to the myelinated conduction, where the action potential plunges much faster (100 m/s) from one node to another. It occurs in myelinated axons, where the flow of ions is discontinuous because of the uneven distribution of voltage-gated channels.
Q.4 Explain GFR
Glomerular Filtration
- Glomerular filtration is a critical renal process wherein blood is filtered in the kidneys through tiny clusters of looping blood vessels known as glomeruli. The glomerular filtrate is created when soluble materials from the bloodstream, such as salts, water, and waste items, are transferred into the kidney tubules as part of this filtration mechanism.
- As blood flows through the glomerulus protein-free plasma filters through the glomerular capillaries into Bowman’s capsule
- This process is known as glomerular filtration which is the first step in urine formation.
Glomerular Filtration Rate (GFR)
- The rate at which plasma is filtered by the kidney glomeruli.
- An important measurement in the evaluation of kidney function
- GFR = 125 mL plasma/min or, 180 L/day
- Plasma volume (70-kg young adult man) = about 3L, the kidneys filter the plasma some 60 times in a day.