Valvular Heart Disorders
Introduction
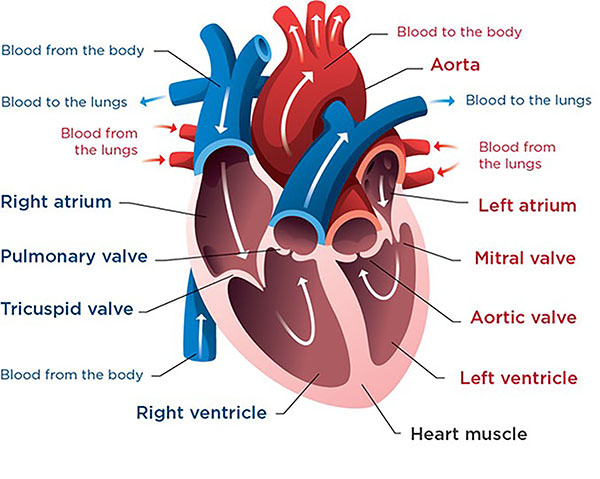
The movement of blood through the heart is crucial for human life. But in addition to perfusion , blood must flow through the heart in an efficient and orderly manner. So here we will focus on the cardiac disorders that affect the structure of heart and impair the efficiency of the heart as a pump.
Definition
- Valvular heart disease can be defined as the damage to or a defect in one of the four heart valves - tricuspid, bicuspid (mitral), pulmonary, and aortic.
Some important terms -
1. Regurgitation- The valve’s tissues flaps (leaflets ) do not fully close or the edges do not fully meet, which causes blood to leak back into the heart.
2. Stenosis- The leaflets can not have an opening for blood to flow through.
3. Atresia- The heart valves do not have an opening for blood to flow through.
Incidence
- Valvular heart diseases remain fairly common in United States even through the incidence is steadily decreasing as the incidence of rheumatic fever decreases
- Mitral valve prolapse syndrome is one of the most common cardiac abnormalities as much as 5% of the population is affected , and females are affected more often than males.
Congenital Valvular Disease
These occur when a valve does not form correctly in the developing fetus, although it can be diagnosed at any age. Mostly affected valves are pulmonary and aortic.
It is of four types-
- Pulmonary atresia
- Pulmonary stenosis
- Tricuspid atresia
- Bicuspid aortic valve disease
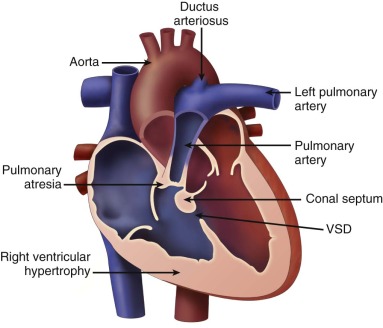
1. Pulmonary atresia
- Pulmonary atresia is a congenital birth defect, in which pulmonary valve does not form properly.
- In this, a solid sheet of tissues form at place of valve opening , so valve stays closed. So due to this blood can not go to lungs from right ventricle to pick up oxygen.
Cause-
- Idiopathic.
- It can be linked with another type of congenital heart defect (Patent Ductus Arteriosus).
- It can occur with or without ‘Ventricular septal defect’
Symptoms-
- Usually occur in the first few hours of life , although it may take up to few days .
- Bluish colourd skin (cyanosis).
- Fast breathing.
- Fatigue.
- Poor feeding habits.
- Shortness of breath.
Investigations
- Chest X ray.
- Echocardiogram.
- Electrocardiogram.
- Heart catheterization.
- Pulse oximetry.
Treatment-
- Prostaglandin E1 this medicine keeps blood vessel (PDA) open b/w pulmonary artery and aorta.
- Heart Catheterization.
- Open heart surgery
- To repair or replace valve
- To place a tube b/w right ventricle and pulmonary artery.
4. Reconstriction of heart as a single ventricle (for temporary period).
5. Heart transplant.
Complications
- Delayed growth and development.
- Seizures.
- Stroke.
- Infectious endocarditis.
- Heart Failure.
- Death.
2. Pulmonary stenosis
- Pulmonary stenosis or narrowing occurs when the valve can not open wide enough leading to obstructed blood flow from right ventricle to pulmonary artery.
Causes-
- Idiopathic.
- Congenital.
- Due to problems during Intra uterine life.
- Defect occur alone or with other heart defects.

Symptoms-
- Most cases are mild with no symptoms.
- Presence of heart murmur sound in infants during routine examination.
- When the valve stenosis is moderate to severe , the symptoms are-
- Abdominal distension.
- Cyanosis in some clients.
- Poor appetite
- Chest pain.
- Fainting.
- Poor weight gain or Failure to thrive in infants with a severe blockage.
- Sudden Death.
Investigations-
- Physical Examination ( presenting heart murmur sound) .
- Other tests are
- Cardiac catheterization,
- Chest X-ray,
- ECG,
- Echocardiogram,
- MRI of Heart.
Treatment:-
- No need of treatment for mild cases.
- In Case of other associated heart defects, the drugs may be used
- Prostaglandin.
- Blood thinners.
- Diuretics.
- Antiarrythmic drugs.
3. Vulvoplasty (percutaneous balloon pulmonary dilation) may be performed in absence of other heart disease.
4. Valve repair or replacement.
Complications -
- Abnormal heart beats (arrythmias).
- Heart failure & right sided heart enlargement.
- After repair the chances of pulmonary regurgitation.
- Death.
3. Tricuspid atresia
- In this condition the tricuspid valve is missing or abnormally developed . This defect blocks the blood flow from right atrium to right ventricle.
Causes-
- Idiopathic.
- Heredity.
- Risk factors are down’s syndrome.
Symptoms
- Cyanosis.
- Tacypnea.
- Fatigue.
- Poor growth
- Shortness of breath.
Investigations-
- By routine pre natal Ultrasound imaging or by post natal examination (signs of cyanosis).
- Physical examination often showing the presence of heart murmur sound at birth and may increase in loudness over several months
- Tests are- ECG, Echocardiogram, Chest X-ray , Cardiac catheterization and MRI of heart.
Treatment-
- Prostaglandin E1 is administered to keep ductus arteriosus open (so that blood can circulate to lungs).
- This condition always require surgery-
- An artificial shunt is inserted to keep blood flowing to lungs (in some cases it is not needed).
- Glenn-shunt or hemi-fontan procedure (in this half of veins carrying blue blood from upper half of body directly to pulmonary artery),( at age of 4-6 months). ( during first & second stage child may still look cyanotic )
- This is final step also called Fontan procedure ( in this the rest of veins carrying blue blood from body are connected directly to pulmonary artery leading to lungs. The left ventricle is now only has to pump to body, not to lungs),(at the age of 18 months to 3 years). (after this final step the baby is no longer cyanotic)
Complications-
- Arrythmias.
- Heart failure.
- Ascites (fluid in abdomen) ,and Pleural effusion (fluid in lungs).
- Blockage of artificial shunt.
- Stroke or other neural disease.
- Sudden death.
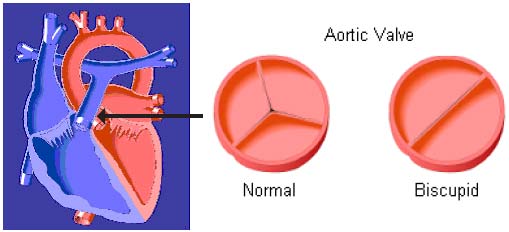
4.Bicuspid aortic valve disease
- In this condition the aortic valve has only two cusps or leaflets instead of three. Bicuspid aortic valve works normally for years without any signs of problem, but the valve does not function well.
Causes
- Idiopathic.
- Latest studies suggest that BAV is caused by a connective tissue disorder that also causes other circulatory problems
- Often associated with coarction of aorta (narrowing of aorta).
Symptoms
Most of time symptoms are absent in infants and children, however abnormal valve can leak or narrow overtime the symptoms are-
- Tiredness
- Chest pain
- Difficulty in breathing
- Palpitations
- Loss of consciousness
- Pale skin.
Investigations
1. Physical examination presenting-
- Enlarged heart
- Heart murmur
- Weak pulse in wrist and ankles.
2. MRI of heart.
3. Echocardiogram.
4. If complications or additional heart defects are suspected ,tests adviced are-
- Chest X-ray
- ECG
- Cardiac catheterization.
Treatment-
- In severe conditions the surgery to repair or replace a leaky or narrowed valve.
- Vulvoplasty (a catheter with a balloon attached at its tip is inserted in groin and directed to heart , the balloon is inflated to make aortic valve larger).
- Medicines may be needed to relieve symptoms
- Beta blockers, ACE inhibitors (to lower workload on heart)
- Water pills.
Complications-
- Heart failure.
- Leakage of blood through valve back in to heart.
- Narrowing of valve’s opening.
- Aortic valve or cardiac muscle infection.
Acquired Valvular Disease
- The valves that are formed properly at birth can still develop problems related to aging, infection ,heart attack or heart damage and other events that cause wear and tear to valves.
- Valve function can also be affected by a build up of calcium deposits on the valve leaflets , making them stiff and inflexible. ( mostly affected valves are aortic and mitral)
A. Disorders of mitral valve include-
- Mitral valve prolapse
- Mitral stenosis
- Mitral regurgitation
B. Disorders of aortic valve include-
- Aortic stenosis
- Aortic regurgitation
A. Disorders of mitral valve include
1. Mitral valve prolapse
It is also called-
- Barlow syndrome.
- Myxomatous valve syndrome.
- Click murmurs syndrome.
- Mitral valve prolapse is a condition in which the two valve flaps of mitral valve do not close smoothly, but insteatd bulge (prolapse) upward in left atrium that may cause heart murmur.
- It is the stretching of the valve leaflet into the atrium during - systole. Incidence is higher in women than in men.

Causes-
- Abnormally stretched valve leaflets (myxomatous degeneration)
- Genetic risk of developing MVP
- Can be due to other connective tissue disease.
- Other causes include-
- Ethlers- danlos syndrome (a group of connective tissue disorders).
- Marfan syndrome (a genetic disorder of connective tissue).
- Rheumatic heart disease
- Ischemic papillary muscle dysfunction.
Pathophysiology
Pathophysiology of mitral valve prolapse is-
Mitral valve leaflet ➡️Atrium➡️Ballooning➡️Stretching of the leaflet➡️Valve is not closed
➡️Blood regurgitation from Lt. ventricle back into the Lt. atrium
Symptoms-
Initially no symptoms seen.
But in later stages symptoms may be-
- Palpitation
- Shortness of breath
- Cough
- Fatigue (tiredness)
- Anxiety
- Chest discomfort/Chest Pain
- Tachycardia
Investigations-
Physical examination may reveal- Heart murmur
Client may need other tests to diagnose MVP-
- Echocardiography
- Doppler USG
- Chest X-ray
- ECG.
Treatment-
1. Goals of treatment may include-
- Correcting underlying mitral valve problem.
- Preventing infective endocarditis, arrythmias, etc.
- Relieving symptoms.
2. Drugs including
- Beta blockers (labetalol) to treat palpitation and chest discomfort.
- Blood thinners (to treat atrial fibrillation).
- Diuretics.
- Antiarrhythmics (flecainide and procainamide).
- Vasodilators (isosorbide dinitrate and hydralazine).
3. Surgery including valve repair and replacement.
2. Mitral stenosis
- In this condition the the valve does not open fully due to its narrowing, that restricts the flow of blood.
- It is an obstruction of blood flowing from the left atrium into left ventricle.

Causes-
- Rheumatic fever (causes fibrosis or thickening of mitral valve).
- Severe mitral leaflet calcification.
- Congenital absence of one of the papillary muscles.
- Endocardial vegetation (may cause ulceration and perforation of heart valve cusps).
- Congenital mitral valve defect.
- Tumors.
- Rheumatoid arthritis.
- Systemic lupus erythematosus (a chronic autoimmune disease)
- Rheumatic endocarditis.
Pathophysiology
Pathophysiology of mitral stenosis is-
Marked stenosis➡️Opening narrows➡️Difficulty of moving blood from left atrium to left ventricle➡️Increased blood volume➡️Left atrium dilates and hypertrophies➡️As no valve protects the pulmonary vein circulation➡️Backflow of blood from atrium occurs➡️Pulmonary circulation congestion➡️Ventricle contract with high pressure➡️Excessive stress occurs➡️Right ventricle fails
Symptoms-
- Adults may have no symptoms.
- However symptoms get worse with exercise or other activity. Mostly between 20-50 yrs of age.
- Symptoms are
- Chest discomfort (extended to arm , neck, jaw, etc.)
- Cough, dyspnea, fatigue.
- Respiratory infections.
4. In infants and children within 2 yrs of life-
- Cough.
- Poor feeding.
- Sweating while feeding.
- Poor growth
- Shortness of breath.
Investigations-
1. Physical examination may reveal-
- Heart murmur sound or other abnormal sound.
- Arrythmias.
2 Other test may include-
- Chest X-ray.
- CT scan of heart.
- Echocardiogram.
- ECG.
- MRI of heart.
- Transesophageal echocardiogram (TEE).
Treatment-
1. Initially symptomatic management.
2. Drugs to treat symptoms of heart failure , hypertension and arrythmia include-
- Diuretics
- Nitrites
- Beta blockers
- Calcium channel blockers
- ACE inhibitors.
3. Anticoagulants (blood thinners).
4. Antibiotics (penicillin).
5. Surgeries needed
- Percutaneous mitral balloon valvotomy (vulvoplasty).
- Valve replacement.
Complications-
- Atrial fibrillation and atrial flutter.
- Stroke.
- Congestive heart failure.
- Pulmonary edema.
- Pulmonary hypertension.
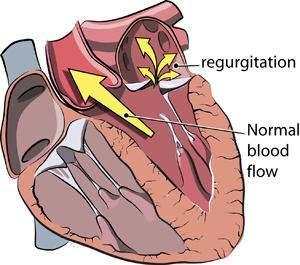
3.Mitral regurgitation
- It is the leakage of blood backward through mitral valve each time the left ventricle contracts.
- It occurs when blood from left ventricle is ejected back into the left atrium during systole.
Causes-
1. It may begin suddenly, often occurs after heart attack.
2. Due to weakening or damaging of valve or heart tissue arround the valve.
3. Risk factors are-
- Coronary Artery Disease (CAD) and hypertension
- Valvular infections
- Mitral valve prolapse
- Untreated syphilis (rarely)
- Rheumatic heart diseases (rarely)
Clinical Manifestations
1. Asymptomatic
2. When cardiac output falls, it may lead to-
- Fatigue and dyspnea
- Cough
- Orthopnea
- Tachypnea
- Paroxysmal nocturnal dyspnea
- Peripheral edema
3. Palpitation, shortness of breath on exertion from pulmonary congestion.
Investigations-
1. Physical examination may reveal
- A thrill (vibration) sound over the heart.
- A heart murmur sound
- Crackles in lungs (if fluid backs up into lungs)
- Hepatomegaly
2. Some tests may be done
- CT scan of chest
- Echocardiogram (transthoracic or transesophageal)
- MRI.
Treatment-
- Symptomatic treatment.
- Restrict physical activities
- Reduce sodium intake
- Promote sodium excretion with diuretics
- When the symptoms get worse , the following antihypertensive drugs may be prescribed by physician
- Beta blockers (labetalol), ACE inhibitors (captopril), calcium channel blockers (amlodipine).
- Blood thinners(anticoagulants)
- Antiarrythmic drugs
- Water pills (diuretics) (to remove excess fluid in lungs)
6. Client may need surgery if conditions are not treated by drugs (repair or replacement of valve).
Complications-
- Arrythmias
- Valvular infection
- Heart failure.
B. Disorders of aortic valve include-
- Aortic stenosis
- Aortic regurgitation
1. Aortic Stenosis
- It is the obstruction to the forward flow of blood during systole from the left ventricle into the aorta and systemic circulation.
Etiology
- Congenital defects of aortic valve
- Two degenerative processes-
- Calcification of the valve
- Retraction and stiffening of valve from rheumatic fever
Pathophysiology
Pathophysiology of aortic stenosis is-
Orifice of aortic valve narrows➡️Decreased blood flow from left ventricle to aorta➡️Pressure in left ventricle rises➡️Dilation & hypertrophy of ventricle occurs➡️Inadequate cardiac output➡️Increased left ventricle end diastolic pressure➡️Decreased cardiac output and increased pulmonary hypertension
Clinical Manifestations
- Many are asymptomatic
- Exertional dyspnea caused by left ventricular failure
- Dizziness and fainting syncope
- Angina pectoris
- Low pulse pressure
- Palpitations
- Visual disturbances
Diagnostic Evaluation
- A loud rough systolic murmur heard over the aortic area.
- ECG, Echo show → left ventricular hypertrophy
- Left sided heart catheterization → to measure the severity of valvular abnormality
- Pressure tracings are taken from left ventricle and the basis of aorta
- Systolic pressure in left ventricle is higher than that in the aorta during systole.
Management
- Antibiotic prophylaxis
- Digitalis and diuretics for ventricular failure
- Surgical replacement of aortic valve
Nursing Considerations
1. Hemodynamic monitoring- The Nurse should monitor the patient for shortness of breath, angina, hypoxia, and alterations in blood pressure, heart rate or rhythm.
2. Cardiac assessment- Check the patient for a strong apical beat, a weak or delayed carotid pulse, lateral and inferior displacement of the heart's apex, an ejection click, or a low-pitched, harsh, systolic murmur radiating to the neck.
3. Oxygen therapy- Utilize pulse oximetry, arterial blood gases, and mixed venous oxygen saturation to monitor the patient's oxygen saturation.
4. Fluid status- Monitor the patient for the signs and symptoms related to pulmonary congestion and peripheral edema. Restrict prolonged period of nothing by mouth before test to prevent dehydration. Assess fluid volume status by measuring daily weights and intake, output status of the patient.
5. Thromboembolic events- Monitor patients with atrial fibrillation or severely compromised left ventricular function for therapeutic anticoagulation. Patient would be kept on lifelong anticoagulation therapy after a mechanical valve replacement.
Nursing Considerations of Patients on Digitalis
- Monitor apical pulse for 1 minute before administering-Hold dose if pulse <60 in adult or <90 in infant; retake pulse in 1 hour. If adult pulse remains <60 or infant <90, hold drug and notify prescriber. Note any change from baseline rhythm or rate.
- Check dosage and preparation cautiously.
- Avoid IM injections, which may be very painful.
- Follow diluting instructions cautiously, and use diluted solution promptly.
- Avoid giving with meals; this will delay absorption.
- Have emergency equipment ready- have K+ salts, lidocaine, phenytoin, atropine, and cardiac monitor readily available in case toxicity develops.
- Warning: Monitor for therapeutic drug levels: 0.5-2 ng/mL
Points for Patient Education
- Do not stop taking this drug without notifying the health care provider.
- Take pulse at the same time each day, and record it on a calendar. Inform the doctor in case of pulse variation
- Weigh yourself every other day with the same clothing and at the same time. Record this on the calendar.
- Do not start taking any prescription or over the counter products without talking to health care provider. Some combinations may cause drug to drug interactions and increase the risk of digoxin toxicity.
- Wear or carry a medical alert tag stating that you are on this drug.
- Have regular medical checkups, which may include blood tests, to evaluate the effects and dosage of this drug and the drug levels, whether are in therapeutic or toxicity levels.
- Report any unusual slow pulse, irregular pulse, rapid weight gain, loss of appetite, nausea, diarrhea, vomiting, blurred or "yellow" vision, unusual tiredness and weakness, swelling of the ankles, legs or fingers, difficulty breathing.
2. Aortic Regurgitation
- Also called aortic insufficiency.
- It is the failure of aortc valve leding to back flow of blood into left vetricle from aorta during diastole.
Causes
- In past , the rheumatic fever was the main cause for this but the use of antibiotics to treat strep infections made rheumatic fever less common.
- Other causes are-
- Arthritis of spine
- Aortic dissection (its tearing) .
- Congenital valve problems.
- Syphilis.
- Systemic lupus erythematosus.
- Chest trauma.
Pathophysiology
Pathophysiology of aortic regurigitation is
During diastole➡️Blood from aorta returns to left ventricle➡️Blood is delivered from left atrium to left ventricle➡️Left ventricle dilation (as trying to increased volume of blood)➡️Hypertrophy occurs (to increase muscle strength to expel more blood)➡️Increased systolic blood pressure➡️Reflex vasodilatation (arteries attempt to compensate high pressure)➡️Peripheral arterioles relax➡️Decreased peripheral resistance and decreased blood pressure
Symptoms-
- Most common in men (between 30-60 yrs).
- Bounding pulse (strong pulse).
- Chest pain similar to angina.
- Fainting.
- Fatigue.
- Palpitations
- Shortness of breath.
- Swelling of feet , leg, or abdomen.
- Weakness with activity.
Investigations-
1. Physical examination reveal-
- Heart murmur
- Palpitation
- Hard pulses in arms and legs
- Low diastolic B.P.
- Signs of fluid in lungs
2. Aortic insufficiency may be seen on tests
- Aortic angiography.
- Echocardiogram.
- Left cardiac catheterization.
- MRI of heart.
- Transthoracic echocardiogram (TTE), or Transesophageal echocardiogram (TEE).
- Chest X-ray may show swelling of left ventricle.
Treatment-
- No treatment needed in case of no or mild symptoms (but proper checkup is needed).
- Anti-hypertensives.
- Diuretics.
- Limiting activity needed.
- Surgery to repair or replace the aortic valve is to be done.
Complications-
- Arrythmia.
- Heart failure.
- Infection in heart.
Nursing Responsibility
- History taking
- Physical examination (timely).
- Administer drugs as prescribed by physician.
- Monitor for adverse and side effects of drugs administered.
- Teach the client about the complications and treatment plan.
- As doctors prescription the antibiotic therapy is provided before any invasive procedures.
- The nurse teaches the client and his family members about the complication after infections.
- The nurse teaches the patients about to weigh daily and report to doctor if there is a weight gain of more than 2.3 kg in one week.
- Assist the patient to adopt life style modifications.
- If the patient have vulvoplasty or valve replacement, teach them about the procedures , anticipated recovery time and complications.