Arteriosclerosis
Arteriosclerosis
- From the Greek Arterio, meaning artery, and sclerosis, meaning hardening
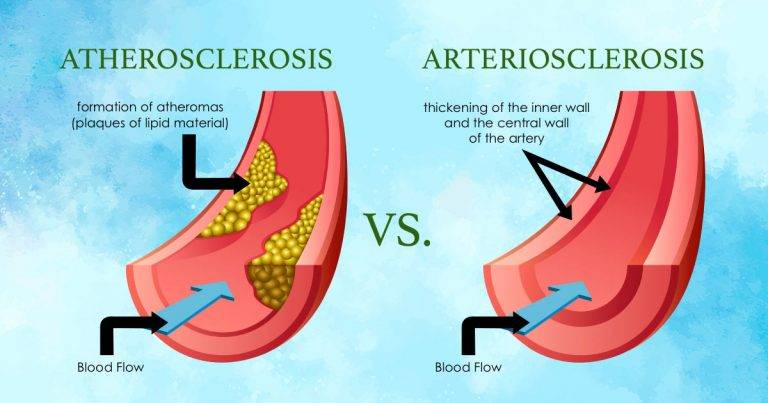
- Arteriosclerosis is the disease of the arteries characterized by thickening, loss of elasticity and calcification of arterial walls. Resulting in decreased blood supply particularly to the cerebrum and lower extremities.
- It is a degenerative process during which elastic tissue is replaced by fibrous tissue mainly tunica media becomes thickened.
- Arteriosclerosis is a general term describing any hardening (and loss of elasticity) of medium or large arteries .
Predisposing Factors
- Heredity- Family history
- Gender- Males are more susceptible than females, until after the female menopause
- Increasing age
- Diabetes mellitus
- Hypertension
- Hyperlipidemia, especially high levels of low-density lipoproteins
- Obesity
- Diet- high in refined carbohydrates and/or saturated fats and cholesterol
- Smoking cigarettes
- Excessive emotional stress
- Sedentary lifestyle
- Excessive alcohol consumption
The following morphologic entities are included under arteriosclerosis-
- Senile arteriosclerosis (affects arteries)-A disorder similar to hypertensive arteriosclerosis, but resulting from advanced age rather than hypertension.
- Hypertensive arteriolosclerosis (affects arterioles)-Hypertensive arteriolosclerosis is a condition where high blood pressure leads to plaque buildup in the arteries, which can result in a stroke or heart attack due to a blockage or a rupture.
- Mönckeberg's arteriosclerosis(Medial calcific sclerosis) (affects arteries)-This condition tends to affect people with diabetes and peripheral arterial disease (PAD), is a type of arterial disease that affects the legs and lower extremities. Some people may refer to this condition as Mönckeberg’s medial calcific sclerosis.
- Atherosclerosis (affects arteries)-This is a common condition in which plaque accumulates in a person’s arteries, attracting immune cells and additional biological debris. This accumulation causes the arteries to harden and narrow.
The last-named, atherosclerosis, is the most common and most important form of arteriosclerosis; if not specified, the two terms are used interchangeably with each other.
Sites of Arteriosclerosis
Arteries in the-
- Brain,
- Kidneys,
- Heart,
- Abdominal aorta
- Legs
Clinical Features
- These depend on the site of affected artery.
- Coronary artery disease cause angina and leads to ischaemia of the cardiac muscle .
- Cerebral artery disease causes ischaemia of the brain and clinical features depend on the area of the brain affected .
- Vertebral artery disease may cause dizziness , faintness or impaired vision.
- The iliac, femoral and popliteal arteries are commonly affected, and the clinical features r as follows-
- Intermittent claudication-Patient complains of severe cramp like pain, commonly in calf muscles, develops during exercise , walking etc. At first the pain ceases when exercise is stopped but as disease progresses the pain is provoked by less exercise and takes longer to subside. It is due to inadequate circulation to meet the demands of working muscles.
- Rest pain-Severe burning pain in foot and toes occurs mostly in night. Patient is frequently wakened by the pain which may be relieved to a certain by the leg being suspended over side of the bed.
- Cold limbs-The toes and feet feel cold both to touch and to the patient.
- Sensory changes-Pin, needle , tingling or complete anaesthesia may be present especially in the hands or feet and is increased by exercise.
- Skin changes-Owing to ischaemia there may be dryness, scaling, brittle nails and loss of hair. Skin may have white shiny appearance or be discolored after blanching. Gangrenous changes resulting in death of tissue may be present in toes or heels.
- Loss of pulses-There may be partial or complete loss of one or more pulses depending on the severity of condition and the site of occlusion.
Pathology
- Degenerative changes begin in the tunica media of medium-sized arteries with destruction of muscle and elastic tissue. These changes spread to affect the tunica intima .
- Calcium is deposited in the tunica media replacing the degenerated tissues.
- Thus there is loss of elasticity which leads to increased peripheral resistance and raised blood pressure.
Diagnostic Evaluation
- Arteriography
- MRI
- CT-scan
- Doppler studies use ultrasound or sound waves
Treatment
To help prevent hardening of the arteries, make the following lifestyle changes-
- Avoid fatty foods. Eat well-balanced meals that are low in fat and cholesterol.
- Include several daily servings of fruits and vegetables.
- Limit alcohol intake.
- Exercise daily.
- Quit smoking-This is the single most important change you can make to reduce your risk of heart disease and stroke.
- Blood pressure checked every 1 - 2 years before age 50 and yearly after age 50. Have your blood pressure checked more often if you have high blood pressure, heart disease, or you have had a stroke.
- If your blood pressure is high, it is important for you to lower it and keep it under control. Blood pressure should be kept below 140/90 mmHg
- Diabetic, kidney disease, or have had a stroke or heart attack, your blood pressure should probably be less than 130/80 mm/Hg
- Wear warm loose clothes.
- Keep skin clean & free from infection or pressure.
- Avoid - Cold, using hot bottles, tight shoes, socks, belts, Sitting with cross legs.
- Analgesics are prescribed to relieve pain.
- Anticoagulants to prevent blood coagulation.
- Medicine for high cholesterol levels if lifestyle changes do not work. This will depend on-
- Age
- Heart disease or other blood flow problems
- Smoker or overweight
- High blood pressure or diabetes.
- Antiplatelet drugs.like Aspirin or another drug called clopidogrel (Plavix) to help prevent blood clots from forming in your arteries.
Surgical Management
Vascular surgical procedures are divided into two groups: Inflow procedures, which provide blood supply from the aorta into the femoral artery, and outflow procedures, which provide blood supply to vessels below the femoral artery.
Surgical Revascularization
- Embolectomy- Removal of emboli
- Thrombectomy- Removal of thrombus
- Endarterectomy- Removal of atherosclerotic plaque from the artery
- Bypass use of vessel graft to route blood flow around blocked area.
Nursing Management
Assessment
The nursing assessment comprises a thorough medical and pharmaceutical history as well as the identification of peripheral artery disease risk factors. The nursing examination may reveal signs and symptoms such as claudication pain, forefoot rest pain, pallor, cyanosis, weak or absent peripheral pulses, and skin disintegration or ulcerations.
Nursing Diagnosis
Based on assessment data, major nursing diagnosis for the patient may include the following-
- Ineffective peripheral tissue perfusion related to compromised circulation
- Chronic pain related to impaired ability of peripheral vessel to supply tissues with oxygen
- Risk for impaired skin integrity related to compromised circulation
- Deficient knowledge regarding self-care activities
Complications
- Aneurysm -Especially in the arc of aorta.
- Rupture of artery from a trivial cause such as a slight blow or injury or a sudden rise in blood pressure.
- Coronary artery disease
- Kidney disease
- Mesenteric artery ischemia
- Peripheral artery disease
- Renal artery stenosis
- Stroke