Leukemia
The word Leukemia comes from the Greek leukos which means "white" and aima which means "blood".
Definition-
- It is a group of malignant disorder, affecting the blood and blood forming tissue of the bone marrow lymph system and spleen.
- Group of malignant disorders affecting the blood and blood forming tissues of the bone marrow, lymph system and spleen.
- Leukemia is a cancer of blood forming cells in the bone marrow.
Due to uncontrolled growth of leukemic cells in the bone marrow, there is inadequate space in the bone marrow for normal blood production.
The lack of normal blood growth results in-
- Lack of normal WBC- risk of infection
- Lack of normal RBC- fatigue, weakness, anemia
- Lack of normal platelets- risk of bleeding
Incidence
- Leukemia accounts for 8% of all human cancers.
- Most common malignancy in children and young adults
Etiology
- Causes exactly not known
- Genetic influence
- Exposure to ionizing radiation and chemicals (benzene)
- Congenital abnormalities, e.g., Down's syndrome.
- Presence of primary immunodeficiency
- Infection with the human T cells leukemia virus type-1 (HTLV-1)
Risk Factors
- Age- Older adults are more likely to develop acute myeloid leukemia
- Smoking:-20% of acute myeloid leukemia cases are linked to smoking.Doubles the risk of disease in people older than 60
- Genetic disorders-Down's syndrome, Fanconi anemia
- High doses of radiation-Long-term survivors of atomic bombs
- Previous chemotherapy treatment-Breast cancer, ovarian cancer, lymphoma
- Exposure to industrial chemicals such as benzene
- Family History
Pathophysiology
- Leukemic cells leave the bone marrow and travel through the circulatory system.
- Infiltration of other body tissues such as the central nervous system, testes, skin, gastrointestinal tract, lymph nodes, liver and spleen.
- Death usually is due to internal hemorrhage.
- Development of leukemia in the bloodstream.
Begins with malignant transformation of a single stem cell.➡️Leukemia cells proliferate slowly➡️Have a prolonged life span and accumulate in the bone marrow➡️As they accumulate, they compete with proliferation of normal cells➡️Leukemia cells do not function as mature WBCs and are ineffective in the inflammatory and immune process➡️Leukemia cells replace normal hematopoietic elements in the marrow➡️Erythrocyte and platelet producing cells are crowded out Severe anemia, splenomegaly and bleeding disorders
Diagnostic Evaluation
- Complete history and physical examination
- Complete blood count
- Lumbar puncture
- X-ray
- MRI and CT scan
Classification
According to the stem cell involvement, leukemia is of two types:
- Lymphoid
- Myeloid
1. Acute Myeloid Leukemia
Acute myeloid leukemia results from a defect in the hemopoietic stem cell that differentiates into myeloid cells, monocytes, granulocytes (neutrophils, basophils, eosinophils), erythrocytes and platelets.
Clinical Manifestations
- Fever and infection from neutropenia
- Bleeding tendencies from thrombocytopenia
- Weakness and fatigue from anemia
- Pain from enlarged liver or spleen
- Hyperplasia of gums
- Bone pain from expansion of marrow
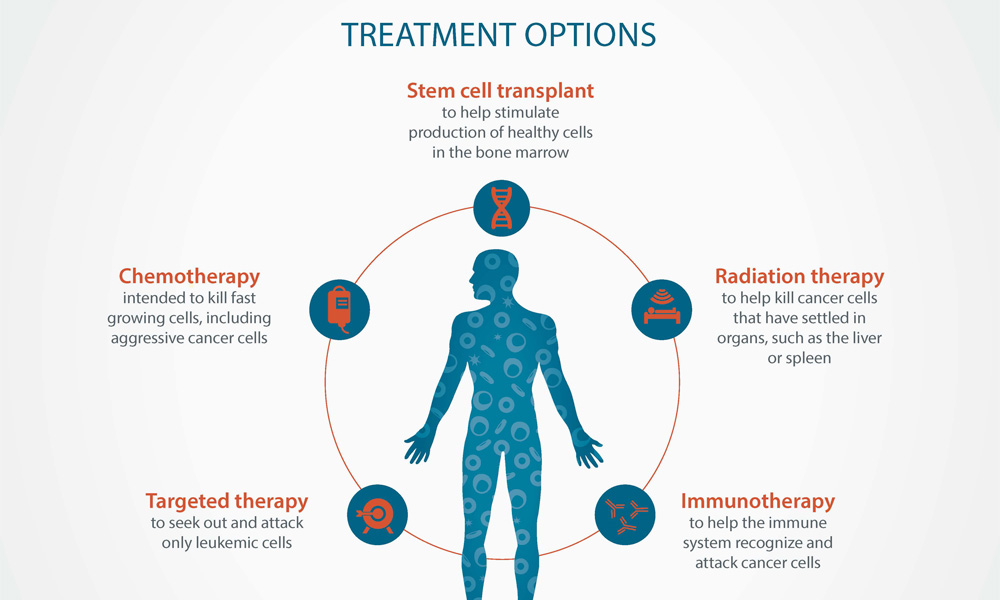
Medical Management
1. Induction Therapy
The aim of induction therapy is to eradicate the leukemic cells, but often causes eradication of normal myeloid cells which causes neutropenia, anemia, thrombocytopenia.
2. Consolidation Therapy
- The consolidation therapy (post remission) is given to eliminate any residual leukemic cells.
- Multiple treatment cycles of various agents are used, e.g., cytarabine.
3. Bone Marrow Transplantation
- Syngeneic bone marrow: Syngeneic marrow is donated by an identical twin. Syngeneic marrow is a perfect HLA match, which eliminates the risk of marrow rejection.
2. Chronic Myeloid Leukemia
Chronic myeloid leukemia arises from a mutation in the myeloid stem cell. Normal myeloid cells continue to be produced, but there is pathologic increase in the production of various forms of blast cells. Therefore, a wide spectrum of cell types exists within the blood, from blast forms through mature neutrophils.
Clinical Manifestations
- CBC-Leukocyte count greater than 100,000/mm
- Short of breath or slightly confused
- Enlarged tender spleen
- Sometimes malaise, anorexia, weight loss
Management
- The aim is to convert the malignant stem cell population back to normal. The agents used are interferon and cytosine, often in combination. These agents are administered daily as subcutaneous injections. This can result in profound fatigue,depression, anorexia, mucositis and inability to concentrate.
- Oral chemotherapeutic agents are used, typically hydroxyurea or busulfan as a less aggressive therapeutic approach focuses on the reduction of the WBC count to a more normal level.
- Leukopheresis can temporarily reduce the number of WBCs. In leukopheresis, the patient's blood is removed and separated, with the leukocytes and the remaining blood returned to the patient.
- If painful splenomegaly develops, then splenectomy is recommended. Bone marrow transplantation can also be done.
3. Acute Lymphoid Leukemia
It results from an uncontrolled proliferation of immature cells (lymphoblast) derived from the lymphoid stem cell. Most common in young children, with boys affected more often than girls.
Clinical Manifestations
- Normal hematopoiesis is inhibited
- Leukocyte count may be high or low but there is always a high proportion of immature cells.
- Leukemic cells infiltration into other organs is more common
- Pain from enlarged liver or spleen and bone pain
- Headache and vomiting because of meningeal involvement.
Management
- Induction therapy: Corticosteroids and vinca alkaloids
- In maintenance phase, lower dose of medications is given for up to 3 years
- Bone marrow transplant.
- Prophylaxis with cranial irradiation or intrathecal chemo- therapy (e.g., Methotrexate).
4. Chronic Lymphocytic Leukemia
Chronic lymphocytic leukemia is a form of leukemia characterized by the proliferation of early B lymphocytes. It is usually discovered when CBC is done as a part of routine physical examinations.
Clinical Manifestations
- Lymphocytosis
- Erythrocytes and platelet count may be normal but in later stages may be decreased
- Lymphadenopathy
- Splenomegaly
- B-symptoms: A constellation of symptoms including fever, drenching sweats (night time) and unintentional weight loss
- Viral infections as herpes zoster
Management
Chemotherapy with corticosteroids and chlorambucil is often used. Cyclophosphamide, vincristine, and doxorubicin are also used.