Placenta Previa
Placenta praevia
- The placenta is partially or totally attached to the lower uterine segment.
- “The placenta is implanted partially or completely over the lower uterine segment (over or adjacent to the internal os) it is called Placenta Praevia”
DEFINITION
In Placenta Praevia the placenta is implanted in the lower uterine segment such that is completely or partially cover the cervix or is close enough to the cervix to cause bleeding when the cervix dilated or the lower uterine segment effaces. (Hull and Resnik, 2009)
INCIDENCE
- About one-third cases of antepartum hemorrhage belong to placenta previa
- 0.5% to 1% of pregnancies.
- It is more common in multiparas and in twin pregnancy due to the large size of the placenta
AETIOLOGY
The exact cause of implantation of the placenta in the lower segment is not known.
- Multiparity
- Increased maternal age (> 35 years)
- Higher altitude
- History of previous scar in the uterus.
- Smoking
- Low implantation of the blastocyst.
- Development of the chorionic villi in the decidua capsularis leading to attachment to the lower uterine segment.
- Large placenta as in twin pregnancy.
TYPES
There are four types of placenta praevia depending upon the degree of extension of placenta to the lower segment.
- Type 1 (Low lying)
- Type 2 (Marginal)
- Type 3 (Incomplete or partial central)
- Type 4 (Central or total)
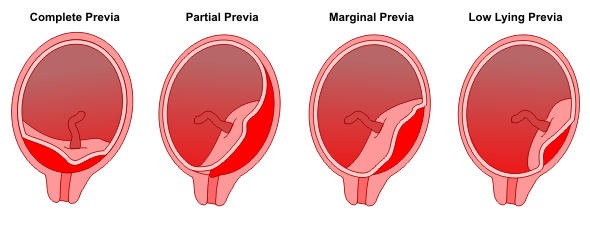
- DEGREES (TYPES)
FIRST DEGREE
-
(Type I = P.P. lateralis = low-lying placenta) The lower edge of the placenta reaches the lower uterine segment but not the internal Os
Second degree
(Type II= P.P. marginals) The lower edge of the placenta reaches the margin of the internal os but does not cover it.

THIRD – DEGREE
(Type III= P.P. incomplete centralis or partial centra)
- Placenta covers part of the cervical os.
- The placenta covers the internal os when it is closed or partially dilated but not when it is fully dilated
4. FOURTH - DEGREE
(Type IV = P.P. complete centralis)-
- Placenta completely covers the os, even when the cervix is dilated.
- The placenta covers the internal os completely whether the cervix is partially or fully dilated.
CLINICAL FEATURES
Symptoms
Vaginal bleeding-
- Sudden in onset, painless
- Revealed bleeding (fresh blood)
- Bright red or dark colored
- Unrelated to activity
Signs-
- General condition and anemia are proportionate to the visible blood loss.
Abdominal examination-
- The size of the uterus
- Uterus feels relaxed and soft.
- The head is floating in contrast to the period of gestation.
- Fetal heart sound is usually present.
- Vaginal inspection- Placenta is felt on the lower segment.
COMPLICATIONS
Complications of Placenta Praevia
1.Maternal complications-
• During Pregnancy
• During labour
• Puerperium
- Fetal complications
During pregnancy
- Antepartum haemorrhage
- Malpresentation
- Premature labour
During labour
- Early rupture of membranes
- Cord prolapses
- Slow dilatation of the cervix
- Intrapartum hemorrhage
Puerperium
- Sepsis
- Postpartum haemorrhage
- Retained placenta
- Subinvolution
Fetal complication
- Low birth weight
- Asphyxia
- Intrauterine death
- Birth injuries
- Congenital malformation
- Maternal and fetal morbidity and mortality
Contrasting Clinical Features of Placenta Praevia and Abruptio Placenta-
| Features | Placenta Previa |
Abruptio Placenta |
|
Vaginal Bleeding |
Minimal to severe, bright red in colour. Painless bleeding, appearing at the end of second trimester, uterus soft, normal tone, observed blood loss comparable to signs of shock |
Moderate dark red in colour Bleeding may or may not be external, uterus rigid, tender and tetanic and shock out of proportion to blood loss. |
| Shock | Unknown | Very common, sudden and profound |
| Abdominal Pain | Absent | Agonizing & unremitting. |
| Location of Placenta | Abnormal–lower uterine segment | Normal–upper uterine segment |
| Associated risk factors | Multiparity, advancing age and uterine |
Maternal hypertension, grand multiparity and hydramnios. |
DIAGNOSIS
Planetography-
- Sonography
- Colour Doppler flow study
- Magnetic resonance
- Vaginal examination
MANAGEMENT
- Prevention
- Immediate management
- Expectant management
- Active management
- Nursing Management
PREVENTION
To minimize the risks, the following guidelines are useful.
- Adequate antenatal care
- Antenatal diagnosis
- Significance of warning hemorrhage
At Home
- Put the patient on bed.
- Abdominal examination
- Vaginal examination must not be done.
Transfer to Hospital -
• Admission to Hospital
TREATMENT ON ADMISSION
- Immediate attention
- Formulation of the line of treatment
1. Immediate attention
• To ensure an adequate blood supply to a women and fetus place the women immediately on bed rest in a side lying position.
• A large bore IV cannula is sited and infusion of normal saline
• Gentle abdominal palpation
2. FORMULATION OF THE LINE OF TREATMENT
The definitive treatment depends upon the duration of pregnancy, fetal and maternal status and extent of the hemorrhage
- Expectant management
- Active (Definite) management
Expectant management
The expectant treatment is carried upto 37 weeks.
Aim- The aim is to continue pregnancy for fetal maturity without compromising the maternal health.
Indications-
- No active bleeding
- Duration of pregnancy is less than 37 weeks
- Patient stable haemo-dynamically
- FHS- good
- Fetal well-being is assured
Conduct of expectant treatment
- Bed rest
- Investigations— like hemoglobin estimation, blood grouping and urine for protein are done.
- Periodic inspection of valval pads
- Supplementary hematinic if patient is anemic
- Use of tocolytics.
- Rh immunoglobulins to all Rh-negative women.
Active management
Indications
- Bleeding occurs at or after 37 weeks of pregnancy
- Bleeding is continuing and of moderate degree
- Patient is in labour
- FHS- absent
- Gross fetal malformation
- Dead fetus
Cesarean delivery is done for all women with sonographic evidence of placenta previa where placental edge is within 2 cm from the internal os. It is especially indicated if it is posterior or thick.
Vaginal delivery
may be considered where placenta edge is clearly 2–3 cm away from the internal cervical os (based on sonography).
NURSING MANAGEMENT
Nursing Diagnosis Decreased cardiac output related to blood loss as manifested by increase in heart rate.
Interventions
- Monitor Vital Signs
- Provide adequate rest &
- Reposition client
- Encourage relaxation techniques
- Elevate Hb of the client
- Encourage use of relaxation Techniques
Ineffective tissue perfusion related to decrease in Hb in blood as manifested by dyspnea.
Interventions
- Monitor Vital Signs.
- Encourage quiet & restful environment.
- Encourage use of relaxation techniques.
- Provide supplemental oxygen to the client as prescribed by the physician.
Deficient fluid volume related to Blood Loss as manifested by vital signs changes.
Interventions-
- Monitor Vital Signs
- Monitor FHR.
- Initiate IV fluids as ordered by the physician.
- Place the patient in left lateral position.
Fear related to outcome of pregnancy as manifested by facial expressions of the mother.
Nursing Interventions
- Assess fetal heart sounds.
- Allow the mother to share her feelings.
- Answer the mother’s questions honestly.
- Include the mother in the planning of the care plan for both the mother and the baby.