Ectopic Pregnancy
Pregnancy-
Pregnancy is the period during which a woman carries a developing fetus normally in the uterus, starting from conception until the baby born.
Normal pregnancy Implantation-
The embryo proceeds through the isthmus to the uterine cavity from up to 72 hours, by the sixth day it enters the uterus and begin to penetrate the decidua(endometrium) this is called Implantation which take place within the uterine cavity in normal position pregnancy.
Ectopic Pregnancy-
Definition-Any pregnancy where the fertilised ovum gets implanted and develop in a site other than normal uterine cavity.
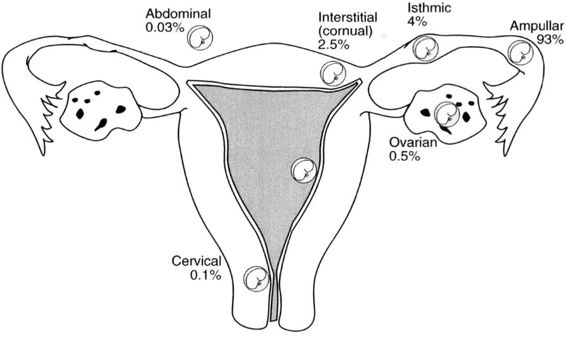
This is a nonviable pregnancy. The majority of ectopic pregnancies occur in the fallopian tube (>90%) but the fertilized ovum can also implant in the ovary, cervix, or abdominal cavity.
- Fallopian tube -95-99%
- Ovarian-About0.5%
- Abdominal-About 0.1%
- Heterotopic pregnancy-Rare case of ectopic pregnancy 1/1000, there may be two fertilized eggs, one outside the uterus and the other inside.
Also called extrauterine pregnancy, is when a fertilized egg grows outside a woman’s uterus.
The classic symptoms are-
- Abdominal pain
- Delayed menses
- Vaginal bleeding or spotting 6 to 8 weeks after the last menstrual period
Risk Factors for Ectopic Pregnancy -
- Tubal corrective surgery
- Smoke cigarettes
- Are older than 35
- Prolonged infertility
- Have a sexual Transmitted Infection
- Tubal sterilization
- Previous ectopic pregnancies
- In utero diethylstilboestrol exposure
- Intrauterine device
- Pelvic inflammatory disease
- Assisted reproduction
- Prior Induced abortion
- Endometriosis
Tubal Pregnancy
Pathophysiology-
- The trophoblast develops in the fertilized ovum and invades deeply into the tubal wall.
- Following implantation, the trophoblast produces HCG with maintains the corpus luteum.
- The corpus luteum Produced Oestrogen and progesterone which change the secretory endometrium into decidua. The uterus enlarges up to 8 weeks and become soft
The tubal pregnancy does not usually proceed beyond 8-10 weeks due to-
- Lack of decidual reaction in the tube
- The thin wall of the tube
- The inadequacy of the tubal lumen
- Bleeding in the site of implantation as trophoblast invades
- Separation of the gestational sac from the tubal wall leads to its degeneration, and fall of HCG level, regression of the corpus luteum and subsequent drop in the oestrogen and progesterone level.
- This leads to separation of the uterine decidual with uterine bleeding
Fate of tubal pregnancy-
- Tubal Mole
- Tubal Abortion
- Tubal Rapture
Tubal Mole-
- The gestational sac is surrounded by a blood clot and retained in the tube.
- This may remain for long period in the tube and from so called (Chronic ectopic pregnancy), or they may be gradually absorbed (Involution)
Tubal Abortion
- This occurs more if ovum had been implanted in the ampullary portion of the tube.
- Separation of the gestational sac is followed by its expulsion into the peritoneal cavity through the tubal ostium.
- If expulsion was complete the bleeding usually ceases but it may continue due to incomplete separation or bleeding from the Implantation site.
Tubal Rapture-
- More common if implantation occurs in the narrower portion of the tube which is isthmus.
- Rupture may occur in the Anti-mesenteric border of the tube-Usually profuse bleeding occurs-Intraperitoneal haemorrhage.
- If rapture occurs in the mesenteric border of the tube, broad ligament haematoma will occur.
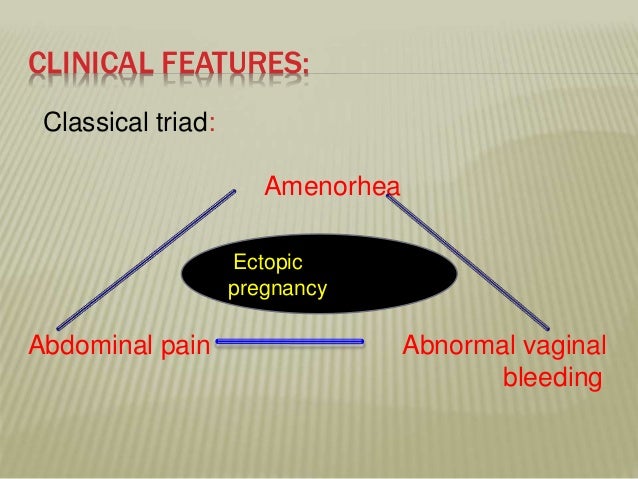
Clinical traid (3As)
- Amenorrhea
- Abdominal pain
- Abnormal vaginal bleeding
Abdominal pain-
- In the lower back, abdominal, or pelvis
- Usually unilateral
- Pina may be confused with a strong stomach pain, it may also feel like a strong cramp
- Shoulder pain- This is caused by free blood tracking up the abdominal cavity and irritating the diaphragm, and is an ominous sign
- Pain while urinating
- Pain while having a bowel movement
Abnormal vaginal bleeding-
- Vaginal bleeding usually mild. An ectopic pregnancy is usually a failing pregnancy and falling level of progesterone from the corpus luteum on the ovary cause withdrawal bleeding.
- Internal bleeding (Hematoperitoneum) is due to haemorrhage from the affected tube
Signs-
General examination-
Sign of early pregnancy (Breast tenderness, nausea and vomiting, change of appetite)
Weakness, pallor, hypotension and tachycardia, tachypnoea due to bleeding
Abdominal examination-
Lower abdominal tenderness and rigidity especially on one side may be present.
- Vaginal examination-
- Vaginal spotting
- Bluish vaginal and bluish soft cervix
- Uterus is slightly enlarged and soft
- Marked pain in one iliac fossa on moving the cervix from side to side
Speculum or bimanual examination-
Should not be performed unless facilities for resuscitation are available, as this may induce rupture of the tube.
Diagnosis-
Detailed History of (cycle, pregnancy. PID, Infertility, Gynaecological surgery, contraception)
Proper general, abdominal, vaginal examination and vital sign
Investigation-
-
- Hormonal assay-
- Serum B-HCG urine pregnancy test are positive in only 50-60% 0f ectopic.
- If test is positive, and double every 36-48 hour till reach 1500 IU/l which is the threshold of discrimination for intrauterine pregnancy, this indicates a normal intrauterine pregnancy
- An abnormal rise in blood B-HCG level may indicate an ectopic pregnancy and ultrasonography is indicated.
- Progesterone-
Generally, a progesterone concentration of greater than 25ng/ml is highly correlated with a normal intrauterine pregnancy while a concentration of less than 5 ng/ml is highly correlated with an abnormal and nonviable pregnancy.
-
- Ultrasound
- Culdocentesis-
- In this test, a needle is insert into the space at the top of the vagina, behind the uterus and in front of the rectum to aspirate fluid and determines if there is blood in the space behind the uterus.
- If non-clotting blood is aspirated from the Douglas pouch, intraperitoneal haemorrhage is diagnosed. But if not, ectopic pregnancy cannot be excluded.
- Laparoscopy or Laparotomy-
An endoscope is insert through a small incision in the woman’s abdomen-
- This allow you to see the fallopian tubes and other organs.
- This take place in an operating room with anaesthesia
Risks for the Woman
Haemorrhage related to rupture of fallopian tube
Decreased fertility related to removal of fallopian tube
Assessment Findings
- Signs and symptoms of ectopic pregnancy are often subtle or even absent
- Irregular vaginal spotting with dull, aching pelvic pain with or without signs of pregnancy
- Hemorrhage
- Positive pregnancy test
- Ultrasound confirmation of ectopic pregnancy
Assessment Findings before Tubal Rupture
- Abdominal pain and tenderness
- Sharp abdominal cramps
- Delayed menses
- Abnormal vaginal bleeding or spotting
Assessment Findings after Tubal Rupture-
- Acute, severe lower abdominal pain and may have referred shoulder pain
- Faintness and dizziness
- Signs of shock (e.g. hypotension, tachycardia)
Medical Management
- Type of surgical management depends on the location and cause of the ectopic pregnancy, and extent of tissue involvement.
- Nonsurgical medical management of ectopic pregnancy may be indicated in hemodynamically unstable women. Methotrexate, a type of chemotherapy agent, will cause dissolution of the ectopic mass.
Ant shock treatment-Ant shock measures are to be taken energetically with simultaneous preparation for urgent laparotomy.
- Ringer’s solution (crystalloid) is started, if necessary, with venesection.
- Arrangement is made for blood transfusion. Even if blood is not available, laparotomy is to be done desperately. When the blood is available, it is better to be transfused after the clamps are placed to occlude the bleeding vessels on laparotomy, as it is of little help to transfuse when the vessels are open.
- After drawing the blood samples for grouping and cross matching, volume replacement with colloids (hemocoel) is to be done.
Laparotomy-
Indications of laparotomy are-
- Patient hemodynamically unstable.
- Laparoscopy contraindicated.
- Evidence of rupture. The principle in laparotomy is “quick in quick out”.
Unruptured tubal Pregnancy-May be
A. Expected- Where only observation is done hoping spontaneous resolution.
B. Medical- Number of chemotherapeutic agents have been used either systemic or direct local (under sonographic or laparoscopic guidance) as medical management of ectopic pregnancy.
C. Surgical-
Indications-
- Cases not fulfilling the criteria of medical therapy.
- Cases where HCG levels are not decreasing despite medical therapy.
- Persistent fetal cardiac activity.
1. Linear Salpingostomy- A longitudinal incision is made on the antimesenteric border directly over the site of ectopic pregnancy. After removing the products (by fingers, scalpel handle or by suction), the incision line is kept open to be healed later on by secondary intention. Haemostasis is achieved by electrocautery or laser.
2. Linear Salpingotomy- The procedures are the same as those of salpingostomy. But the incision line is closed in two layers with 7-0 interrupted vicryl sutures. This is not commonly done.
3. Segmental Resection- This is of choice in isthmic pregnancy. End-to-end anastomosis can be done immediately or at a later date after appropriate counselling of the patient.
4. Fimbrial Expression-This is ideal in cases of distal ampullary (fimbrial) pregnancy and is done digitally.
Salpingectomy - Salpingectomy is the surgical removal of one (unilateral) or both (bilateral) fallopian tubes.

- Whole of the affected tube is damaged,
- Contralateral tube is normal or
- Future fertility is not desired.
Nursing Management
- Offer explanations and reassurance related to the plan of care.
- Provide support related to the pregnancy loss.
- Ensure stabilization of cardiovascular status.