The urinary system
The urinary system is one of the excretory systems of the body. It consists of the following structures-
- 2 kidneys, which secrete urine
- 2 ureters, which convey the urine from the kidneys to the urinary bladder
- 1 urinary bladder where urine collects and is temporarily stored
- 1 urethra through which the urine is discharged from the urinary bladder to the exterior
Organs associated with the kidneys
As the kidneys lie on either side of the vertebral column each is associated with a different group of structures.
Right kidney-
Superiorly - The right adrenal gland
Anteriorly -The right lobe of the liver, the duodenum and the hepatic flexure of the colon
Posteriorly -The diaphragm, and muscles of the posterior abdominal wall
Left kidney-
Superiorly - The left adrenal gland
Anteriorly - The spleen, stomach, pancreas, jejunum and splenic flexure of the colon
Posteriorly - The diaphragm and muscles of the posterior abdominal wall.
Layers of Kidney-
Components of kidney are arranged in three layers.
- Outer cortex
- Inner medulla
- Renal sinus.
1. Outer Cortex
Cortex is dark and granular in appearance. It contains renal corpuscles and convoluted tubules. At intervals, cortical tissue penetrates medulla in the form of columns, which are called renal columns or columns of Bertani.
2. Inner Medulla
Medulla contains tubular and vascular structures arranged in parallel radial lines. Medullary mass is divided into 8 to 18 medullary or Malpighian pyramids. Broad base of each pyramid is in contact with cortex and the apex projects into minor calyx.
3. Renal Sinus
Renal sinus consists of the following structures:
- Upper expanded part of ureter called renal pelvis
- Subdivisions of pelvis- 2 or 3 major calyces and about 8 minor calyces
- Branches of nerves, arteries and tributaries of veins
- Loose connective tissues and fat.

Microscopic structure of the kidney
The kidney is composed of about 1 million functional units, the nephrons, and a smaller number of collecting tubules. The collecting tubules transport urine through the pyramids to the renal pelvis giving them their striped appearance. The tubules are supported by a small amount of connective tissue, containing blood vessels, nerves and lymph vessels.
Nephron-
the structural and functional unit of kidney. Each kidney consists of 1 to 1.3 million of nephrons. The number of nephrons starts decreasing after about 45 to 50 years of age at the rate of 0.8% to 1% every year’
Nephron is formed by two parts
- A blind end called renal corpuscle or Malpighian corpuscle
- A tubular portion called renal tubule.
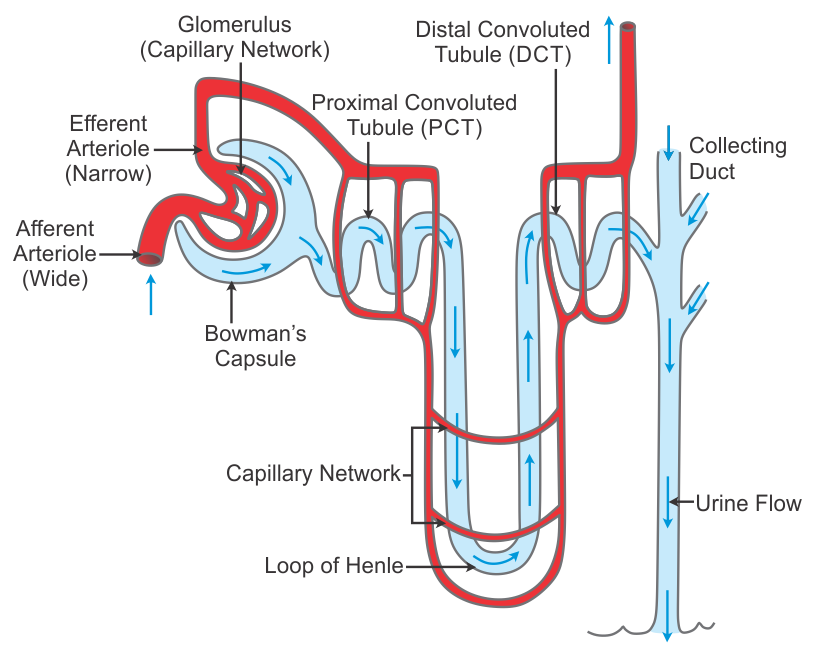
1. Renal corpuscle or Malpighian corpuscle-
Renal corpuscle or Malpighian corpuscle is a spheroidal and slightly flattened structure with a diameter of about 200 µ. Function of the renal corpuscle is the filtration of blood which forms the first phase of urine formation.
Renal corpuscle is formed by two portions-
- Glomerulus
- Bowman capsule
a. Glomerulus-
Glomerulus is a tuft of capillaries enclosed by Bowman capsule. It consists of glomerular capillaries interposed between afferent arteriole on one end and efferent arteriole on the other end. Thus, the vascular system in the glomerulus is purely arterial.
Functional histology-
Glomerular capillaries are made up of single layer of endothelial cells, which are attached to a basement membrane. Endothelium has many pores called fenestrae or filtration pores. Diameter of each pore is 0.1 µ. Presence of the fenestra is the evidence of the filtration function of the glomerulus.
b. Bowman capsule-
Bowman capsule is a capsular structure, which encloses the glomerulus. It is formed by two layers-
- Inner visceral layer
- Outer parietal layer.
Visceral layer covers the glomerular capillaries. It is continued as the parietal layer at the visceral pole. Parietal layer is continued with the wall of the tubular portion of nephron. The cleft like space between the visceral and parietal layers is continued as the lumen of the tubular portion.
Functional anatomy of Bowman capsule resembles a funnel with filter paper. Diameter of Bowman capsule is 200 µ.
Functional histology-
Both the layers of Bowman capsule are composed of a single layer of flattened epithelial cells resting on a basement membrane. Basement membrane of the visceral layer fuses with the basement membrane of glomerular capillaries on which the capillary endothelial cells are arranged.
Epithelial cells of the visceral layer fuse with the basement membrane but the fusion is not complete. Each cell is connected with basement membrane by cytoplasmic extensions of epithelial cells called pedicles or feet.
These pedicles are arranged in an interdigitating manner leaving small cleft like spaces in between. The cleft like space is called slit pore. Epithelial cells with pedicles are called podocytes.
2. A tubular portion called renal tubule-
Tubular portion of nephron is the continuation of Bowman capsule. It is made up of three parts
- Proximal convoluted tubule
- Loop of Henle
- Distal convoluted tubule
A. Proximal convoluted tubule-
Proximal convoluted tubule is the coiled portion arising from Bowman capsule. It is situated in the cortex. It is continued as descending limb of loop of Henle. Length of proximal convoluted tubule is 14 mm and the diameter are 55 µ. Proximal convoluted tubule is continued as loop of Henle.
Functional histology
Proximal convoluted tubule is formed by single layer of cuboidal epithelial cells. Characteristic feature of these cells is the presence of hair like projections directed towards the lumen of the tubule. Because of the presence of these projections, the epithelial cells are called brush-bordered cells.
B. Loop of Henle-
Loop of Henle consists of
- Descending limb
- Hairpin bend
- Ascending limb
Descending limb-
Descending limb of loop of Henle is made up of two segments
- Thick descending segment
- Thin descending segment.
Thick descending segment
Thick descending segment is the direct continuation of the proximal convoluted tubule. It descends down into medulla. It has a length of 6 mm and a diameter of 55 µ. It is formed by brush bordered cuboidal epithelial cells.
Thin descending segment
Thick descending segment is continued as thin descen ding segment. It is formed by flattened epithelial cells without brush border and it is continued as hairpin bend of the loop.
Hairpin Bend
Hairpin bend formed by flattened epithelial cells without brush border and it is continued as the ascending limb of loop of Henle.
Ascending Limb
Ascending limb or segment of Henle loop has two parts-
- Thin ascending segment
- Thick ascending segment.
Thin ascending segment
Thin ascending segment is the continuation of hairpin bend. It is also lined by flattened epithelial cells without brush border. Total length of thin descending segment, hairpin bend and thin ascending segment of Henle loop is 10 mm to 15 mm and the diameter is 15 µ.
Thin ascending segment is continued as thick ascending segment.
Thick ascending segment
Thick ascending segment is about 9 mm long with a diameter of 30 µ. Thick ascending segment is lined by cuboidal epithelial cells without brush border.
C. Distal convoluted tubule-
Distal convoluted tubule is the continuation of thick ascending segment and occupies the cortex of kidney. It is continued as collecting duct. The length of the distal convoluted tubule is 14.5 to 15 mm. It has a diameter of 22 to 50 µ. Functional histology Distal convoluted tubule is lined by single layer of cuboidal epithelial cells without brush border. Epithelial cells in distal convoluted tubule are called intercalated cells (I cell).
Function of Kidney-
Kidneys perform several vital functions besides formation of urine. By excreting urine, kidneys play the principal role in homeostasis.
A. Role in Homeostasis-
Primary function of kidneys is homeostasis. It is accomplished by the formation of urine. During the formation of urine, kidneys regulate various activities in the body, which are concerned with homeostasis such as-
1. Excretion of Waste Products
Kidneys excrete the unwanted waste products, which are formed during metabolic activities-
- Urea (end product of amino acid metabolism)
- Uric acid (end product of nucleic acid metabolism)
- Creatinine (end product of metabolism in muscles)
- Bilirubin (end product of hemoglobin degradation)
- Products of metabolism of other substances.
2. Maintenance of Water Balance
Kidneys maintain the water balance in the body by conserving water when it is decreased and excreting water when it is excess in the body. This is an important process for homeostasis.
3. Maintenance of Electrolyte Balance
Maintenance of electrolyte balance, especially sodium is in relation to water balance. Kidneys retain sodium if the osmolarity of body water decreases and eliminate sodium when osmolarity increases.
4. Maintenance of Acid–Base Balance
The pH of the blood and body fluids should be maintained within narrow range for healthy living. It is achieved by the function of kidneys Body is under constant threat to develop acidosis, because of production of lot of acids during metabolic activities. However, it is prevented by kidneys, lungs and blood buffers, which eliminate these acids.
B. Hemopoietic Function-
Kidneys stimulate the production of erythrocytes by secreting erythropoietin. Erythropoietin is the important stimulating factor for erythropoiesis. Kidney also secretes another factor called thrombopoietin, which stimulates the production of thrombocytes.
C. Endocrine Function-
Kidneys secrete many hormonal substances in addition to erythropoietin and thrombopoietin. Hormones secreted by kidneys
- Erythropoietin
- Thrombopoietin
- Renin
- 1,25-dihydroxycholecalciferol(calcitriol)
- Prostaglandins.
D. Regulation of blood Pressure-
Kidneys play an important role in the long-term regulation of arterial blood pressure by two ways-
- By regulating the volume of extracellular fluid
- Through renin-angiotensin mechanism.
E. Regulation of Blood Calcium level
Kidneys play a role in the regulation of blood calcium level by activating 1,25-dihydroxycholecalciferol into vitamin D. Vitamin D is necessary for the absorption of calcium from intestine.
The ureters
The ureters are the tubes that convey urine from the kidneys to the urinary bladder. They are about 25 to 30 cm long with a diameter of about 3 mm. The ureter is continuous with the funnel-shaped renal pelvis. It passes downwards through the abdominal cavity, behind the peritoneum in front of the psoas muscle into the pelvic cavity.
Structure
The ureters consist of three layers of tissue-
- An outer covering of fibrous tissue, continuous with the fibrous capsule of the kidney
- A middle muscular layer consisting of interlacing smooth muscle fibres that form a syncytium spiralling round the ureter, some in clockwise and some in anticlockwise directions and an additional outer longitudinal layer in the lower third
- An inner layer, the mucosa, lined with transitional epithelium.
Function
The ureters propel the urine from the kidneys into the bladder by peristaltic contraction of the smooth muscle layer. This is an intrinsic property of the smooth muscle and is not under autonomic nerve control. The waves of contraction originate in a pacemaker in the minor calyces.
The urinary bladder-
The urinary bladder is a reservoir for urine. It lies in the pelvic cavity and its size and position vary, depending on the amount of urine it contains. When distended, the bladder rises into the abdominal cavity.
Structure
The bladder is roughly pear-shaped, but becomes more oval as it fills with urine. It has anterior, superior and posterior surfaces. The posterior surface is the base. The bladder opens into the urethra at its lowest point, the neck. The peritoneum covers only the superior surface before it turns upwards as the parietal peritoneum, lining the anterior abdominal wall. Posteriorly it surrounds the uterus in the female and the rectum in the male.
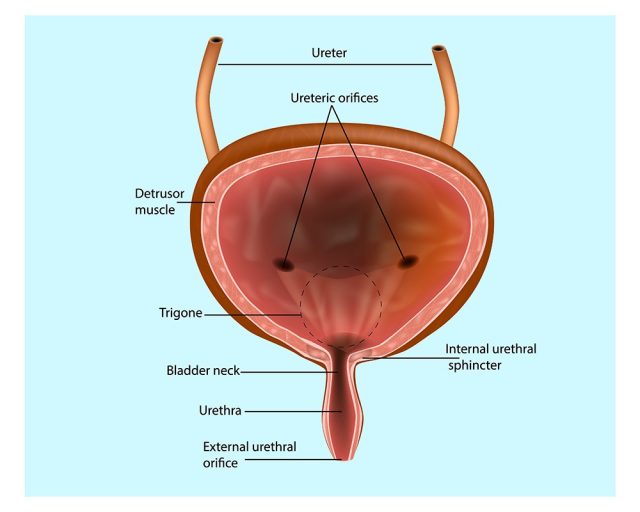
The bladder wall is composed of three layers-
- The outer layer of loose connective tissue, containing blood and lymphatic vessels and nerves, covered on the upper surface by the peritoneum
- The middle layer, consisting of a mass of interlacing smooth muscle fibres and elastic tissue loosely arranged in three layers. This is called the detrusor muscle and it empties the bladder when it contracts
- The mucosa, lined with transitional epithelium
The urethra
The urethra is a canal extending from the neck of the bladder to the exterior, at the external urethral orifice. Its length differs in the male and in the female. The male urethra is associated with the urinary and the reproductive systems.
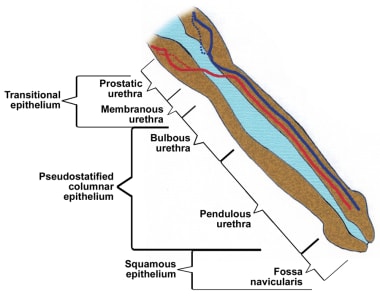
The female urethra is approximately 4 cm long. It runs downwards and forwards behind the symphysis pubis and opens at the external urethral orifice just in front of the vagina.
Its walls consist of three layers of tissue-
- The muscle layer, continuous with that of the bladder. At its origin there is the internal urethral sphincter, consisting mainly of elastic tissue and smooth muscle fibres, under autonomic nerve control. Slow and continuous contraction of this sphincter keeps the urethra closed. In the middle third there is skeletal muscle surrounding the urethra, under voluntary nerve control, that forms the external urethral sphincter
- The submucosa, a spongy layer containing blood vessels and nerves
- The mucosa, which is continuous with that of the bladder in the upper part. In the lower part the lining consists of stratified squamous epithelium, continuous externally with the skin of the vulva.