The third stage of labour
The third stage of labour is that of separation and expulsion of the placenta and membrane. It lasts from the birth of the baby until the placenta is expelled. You will now learn about the physiological changes that take place in this stage of labour.
The third stage of labour starts after the birth of the baby and ends with the expulsion of the placenta, umbilical cords and membranes. Average duration is 5-15 minutes.
Physiological Changes
The physiological changes that take place during this stage, comprises two phases
- The phase of placental separation
- The mechanism of placental expulsion. The control of bleeding also takes place during this period.
Mechanism of Placental Separation
During this phase, the placenta separates from the uterine wall and descends. There are some signs which enables one to know that it has taken place.
The uterine wall contracts and retracts. The upper uterine segment thickens and its capacity reduces. The area of the placental site is diminished; the cotyledons of the placenta becomes compact. Separation begins in the centre or the lower edge of the placenta, at the level of the deep spongy level of the decidua. The process is like the detachment of postage stamps at the perforation between them.
The blood sinuses are torn; a retroplacental clot is formed; the placenta gets detached from the uterus; descends from the lower upper uterine segment into the uterine segment. With the traction, the membranes are peeled off the decidua.
Signs of Placental Separation-
- The uterus becomes globular and contracts firmly
- The uterus rises upward in the abdomen. Changes from discoid to a globular ovoid shape
- The umbilical cord descends 3 inches or more further out of the vagina
- A sudden gush of dark blood from the introitus.
Control of Bleeding
The uterine fibres contracts and retracts as the contraction and retraction of the uterus takes place. They are arranged in three layers, i.e. the outer longitudinal, inner circular and the intermediate, which is the thickest and strongest layer arranged in criss-cross fashion through which the blood vessels run. When the uterus contracts, the blood vessels running through the fibres are occluded, thus controlling haemorrhage. They are also called ‘living ligatures”.
Nature’s Method of Expulsion of Placenta
Nature has two methods of expelling the placenta, described as Schultze and Mathews Duncan.
The Schultze Method
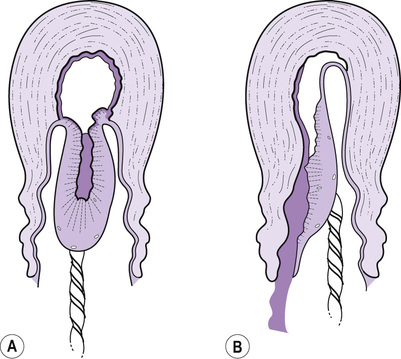
- Is common; occurs in 80% of cases
- Placenta slips into the vagina through the hole in the amniotic sac, like and inverted umbrella.
- Foetal surface appears at the vulva.
- Placental surface is not seen.
- Blood clot is inside the inverted sac.
The Mathews Duncan Method
Occurs in about 20% of deliveries
Placenta slides down sideways and comes through the vulva with the lateral border first. This is like button slipping through a button -hole. The maternal surface is seen and blood escapes.
Nursing Management of Third Stage of Labour
Position of the Woman
This will vary according to the mother’s personal choice, normality of progress and experience of the midwife and the need for monitoring the uterine contractions and blood loss.
Dorsal position-
It enables the mother to cuddle her baby and allow easy palpation of the uterus fundus. The disadvantage is that blood will pool in the vagina.
Upright/kneeling/squatting position-
These positions may be used when the third stage is to be managed passively, but contraindicated following an epidural block.
It is of advantage because it will hasten expulsion of the placenta due to gravity and increased intra-abdominal pressure; aids in observation of blood loss. However, the mother will need support to cuddle her baby.
Observation
You will now learn about the observations to be made in the mother during this stage of labour.
The maternal status needs to be observed. The following observations need to be made by the nurse.
B.P. and Pulse
Blood pressure should be checked periodically. The systolic should be over 110 mm Hg. The pulse is the best guide to the loss of blood. A pulse rate over 90/mt and rising with pallor indicate haemorrhage.
Consistency of the Uterus
The uterus must have the consistency of a firm tennis ball and its shape must be broader laterally than antero-posteriorly. It will feel like a cricket ball when a contraction occurs and between contraction its firm distinct outline should be clearly defined.
Size of the Uterus
After the birth of the baby, the fundus is 2.5 cm above the umbilicus. If it is more than this one should suspect that there is another baby, the placenta is unduly large, blood clots are present in the uterus, or the bladder is full.
Amount of the Blood Loss
The vulva is to be observed for loss of blood. Average amount of blood loss is 120 ml to 240 ml. At times blood loss may not be visible, because clots may form. An increasing pulse rate is indicative of blood loss.
- Level of consciousness
- Respiration: Rate and rhythm
Delivery of Placenta and Membranes
This is done either by active management or by passive physiological management. You will now learn about this management.
Active Management by Controlled Cord Traction
Delivering the placenta by controlled cord traction following the administration of syntometrine 1 ml, at the appearance of the anterior shoulder or after the birth of the head shortens the third stage of labour and reduces blood loss.
Timing of Controlled Cord Traction
After the birth of the baby, usually the placenta should be delivered with the first uterine contraction within 4-5 minutes.
Method of Controlled Cord Traction
Wait for a strong uterine contraction when it is palpably contracting. Place palm of the left hand on the lower abdomen, at the symphysis pubis.
- With the palmer surface, apply counter traction, i.e. brace back the upper uterine segment, the fingers stretching the lower uterine segment, upwards towards the umbilicus to prevent inversion of the uterus.
- With the right hand, grasp the cord.
- Apply traction on the cord in a downward and backward direction, following the line of the birth canal.
- Avoid jerky movements and force.
- Some resistance is felt, but it is important to apply steady tension by pulling the cord firmly and maintaining the pressure.
- If the uterus relaxes, stop traction temporarily. First release the downward traction on the uterus and then the counter traction.
- Then start the same procedure again.
- Once the placenta is visible, cup it in the hand to ease pressure on the membranes.
- Apply gentle upward and downward movement, or twist the placenta. This helps in delivering the membranes intact.

Passive Physiological Management
Before making an attempt to expel the placenta, you ensure that the placenta has separated and is lying in the lower uterine segment.
There are two ways of passively delivering the placenta and membranes. They are :
- Fundal pressure
- Bearing down by the woman
Fundal Pressure
The firmly contracted fundus of the uterus is used as a piston to push out the placenta.
Method-
- Ask the woman to open her mouth and breathe through it slowly and quietly. This helps in relaxation of the muscles.
- Stand on the right side of the woman.
- During a contraction, grasp the fundus with the left hand, positioning the hand in such a way that the fingers are behind the uterus and the thumb is on the anterior surface of the uterus.
- Apply pressure with the palm of the hand in the axis of the pelvic inlet, then in a downward and backward direction.
- With the right hand hold the placenta at the vulva.
- Hold it with both the hands when it is almost completely expelled.
- If the membranes are adherent, turn the placenta round, apply a pair of artery forceps to the membrane and apply gentle traction in an up and down, sideways and circular manner.
Bearing Down
When the placenta has separated and descended and the uterus is contracted, ask the woman to hold her breath and bear down.
Examination of Placenta and Membranes
You need to examine the placenta and the membranes to make sure that no part of it has been retained.
:max_bytes(150000):strip_icc()/169425700-56a770a75f9b58b7d0ea8364.jpg)
Method
The placenta is to be held by the cord allowing the membranes to hang. The hole through which the baby was delivered can be seen. Place a hand and inspect the membrane.
Inspection of Membranes
Weight of the placenta is noted normally placental weight is one-sixth of the baby's weight. The amnion has to be peeled from the chorion, till the umbilical cord to see if the chorion is complete. If not complete, assess the amount of membrane that is missing.
The blood vessels in the membrane should be inspected from its destination. If it runs to a hole in the membrane, it is evident of a retained succenturiate lobe.
Inspection of Maternal and Foetal Surface
- The colour of the placenta – dark bluish red
- The consistency – firm. If it is unhealthy it is soft and mushy if hydrops fetalis is present, it is large, pale, edematous with water oozing from it.
- Cotyledons – all should be present
- Retro – placental clots
- Infarcts i.e. whitish areas
- Position of the insertion of the cord
- Length of the cord
- Blood vessels – Presence of two arteries and one vein is normal.
Care of Mother and Baby
Maternal Comfort and Safety
Some women feel cold and shiver, which is transient. Warmth may be provided by covering with clean dry linen, a blanket and a warm drink.
Care of the Baby
- The baby should be dried, and kept warm with pre-warmed linen or placing an electrically warmed cot mattress.
- The baby can be cuddled by the mother.
- Initiate breast feeding as early as possible.
- Observe general skin colour, respiration and temperature