Normal Puerperium
Normal Puerperium-
Puerperium is period from the expulsion of the placenta to the time the reproductive organs returns to pregravid state lasts 6 weeks'.
Puerperium begins soon after the expulsion of the placenta and normally last for around 6 weeks. generally, we divide this period into-
- Immediate- Within 24 hours
- Early upto 7 Days
- Remote-upto 6 weeks.
Definition
Puerperium is the period following child birth. This is characterized by the following features:
- The generative organs return back approximately to their pregravid state both anatomically and physiologically.
- Lactation is initiated.
- Recuperation from the physical, hormonal and emotional experience of parturition.
"The puerperium is defined as the 6 weeks period commencing after the completion of third stage of labour." -E.M SYMONDS
The puerperium is referring to the 6 weeks period following child birth, when considerable adjustments occur before return to the pre pregnant state.
-PHILIP N. BAKER
It is the period of adjustment after pregnancy and delivery when anatomical and physiological changes of pregnancy are reversed and the body returns to the normal non pregnant state.. (reproductive tract returns to its normal, non-pregnancy state)
This period is also known as post-partum, post-natal, post-delivery period. Puerperium begins as soon as placenta is expelled and lasts for six weeks through the process of involution.
Physiological Changes-
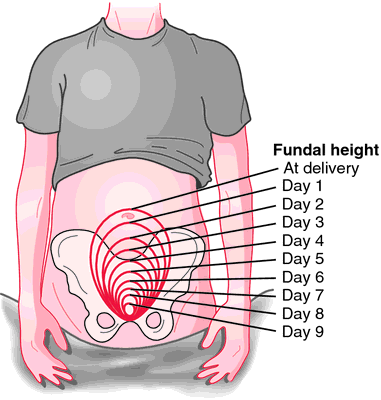
Involution of Uterus
- Involution is the process whereby the pelvic reproductive organs returns to their prepregnant size and position and the placental site of endometrium heals. Failure to complete this process is known as sub-involution.
- After the delivery uterus becomes firm and retracted with alternate hardening and softening. The uterus measures about 20×12×7.5 cms(length, breadth and thickness) and weighs about 1000 gms.
- At the end of 6 weeks it returns to pregravid size of 7.5×5×2.5 cm and weighs 60 gms. This reduction in weight and size is not in the number of cells but also size of the same cells through the process autolysis of the muscle fibres and ischaemia of the uterus.
- The contraction and reduction of the uterine muscle’s fibres compress the bloodvessels and reduce the uterine blood supply.
| Character | Changes |
| Length | From 20 cm to 7.5 cm |
| Breadth | From 12 cm to 5 cm |
| Thickness | From 7.5 cm to 2.5 cm |
| Weight | From 1000gm to 60 gm |
| Placement of uterus after delivery | Fundus of uterus 5cm below the umblicus or 12 cm above symphysis pubis |
| Placement of uterus after 24 hours | At the level of umblicus |
| After one week placement of uterus | 7.5 cm above symphysis pubis |
| After 12 days | Fundus is not palpable |
| Placental site at end of 6 weeks | 1.5 cms |
| Position of uterus | Uterus after 24 hours of delivery reduces at a rate of 1.25 cms (1/2inch) until 11th day |
| Consistency of the uterus | Firm, round hard after delivery |
Reduction of the size-
- After 24 hrs at the level of umbilicus.
- After 1 week 7.5 cms above the symphysis pubis
- 12 days after labour the fundus is not usually palpable.
- The placental site is 7.5 cms and at the end of 6 weeks measures 1.5 cms.
Position of the uterus-
Immediately after delivery the uterus lies midway between the symphysis pubis and the umbilicus. Within 12 hrs, it rises to the level of umbilicus or slightly above it. Uterus begins to descent into the pelvic cavity at a rate of about 1 cm a day until the 10th day, when it may be palpated at or below the level of symphysis pubis.
Consistency of the uterus-
The strong frequent myometrial contractions that control blood flow to the uterus cause it to become hard. Its consistency can be assessed by palpating the uterus. It should feel firm and round. If the fundus is soft, it is called as boggy uterus, indicates that contractions are inadequate allowing blood loss to continue.
Endometrium-
It also undergoes involution after placenta is delivered. The major part of decidua is cast off along with the placenta and membranes, more that the placental sites, only the basal portion of the decidual remains. The superficial part containing the degenerative decidua, blood cells and bits of foetal membrane become necrotic and is cast off in lochia.
Clinical assessment of involution-
- Rate of involution of uterus can be assessed by taking fundal height in relation to symphysis pubis with the measuring tape. Measurement to be taken at the fixed time every day. Bladder and bowel must be emptied, as they may raise the level of fundus.
- Following delivery fundus lies about 13.5 cms about the symphysis pubis. First 24 hours uterus remains constant and then steady decrease in height by 1.25 cms (1/2") in 24 hrs. and by the end of second week uterus becomes a pelvic organ and by six week becomes almost normal in size.
Cervix-
- The cervix contracts slowly.
- It is soft immediately after birth
- After delivery the lower uterine segment and cervix remain loose, thin and stretched. It may also appear odemetous and bruised from the delivery and may have small tears or lacerations.
- It may take few weeks to revert back to normal shape and size of the isthmus.
- By the first post-partum day cervix has sufficiently narrowed and regained its normal consistency to admit two fingers and by the end of first week narrows down to admit the tip of a finger only.
- It admits 2-3 fingers for the first 4-6 days and by the end of 10-14 days is dilated to barely more than 1cm.
- Involution may continue for 3-4 months since the cervix sustained trauma; the parous cervix will never again look like the non-parvous cervix. The external os which previously resembled a dimple, now a slit and laceration may leave scar tissue.
Vaginal Canal
The vaginal canal appears swollen and smooth after delivery, gradually becomes smaller and firm, never regains pre-pregnancy size, rugae partially reappears at third week but never to the same degree as in pregnant size. The introitus remains permanently larger than the vaginal state. The hymen is lacerated and is represented by nodular tags. Occasionally a hematoma may develolp as a result of descent and delivery at external vaginal orifice, vaginal wall at ischial spines and episiotomy site.
Perineum
The perineum muscle is stretched and swollen bruised. The perineum muscle may be intact but still oedematous, erythematous and uncomfortable. A scar may be present if episiotomy was performed.
Ovaries
The ovaries are inactive during the last two trimesters of pregnancy, because of the drop in placental hormones level and gradually resumes the prepregnancy cycle.
Lochia
It is the vaginal discharge for the first fortnight during puerperium. It originates from the uterine body, cervix and vagina.
It contains blood, decidual tissue, epithelial cells from the vagina mucus, bacteria and on occasion, fragments of membranes and small clots. Its odour is fleshy but not offensive. Various types of lochia are-
- Lochia Rubra- The first phase of lochia when discharge is red and bloody called lochia rubra means ‘red’. Lasts from 1-4 days, may contain few small blood clots.it consists of blood, decidual and trophoplastic debris.
- Lochia Serosa- Occurs next 5-9 days, the colour is yellowish pink or pale brownish.it consists of old blood, serum, leukocytes, and tissue debris.
- Lochia-Alba- Pale white because of the presence of leukocytes, lasts from 10-14 days.it consists of leukocytes, decidua, epithelial cells, mucus, and bacteria.
- The colour of lochia indicates the healing stage of the placental site.
- The average amount of discharge for the first 5-6 days is about 250 ml.
Importance of Inspecting Lochia-
- It gives information about the puerperal state of the mother – pads to be inspected daily.
- Odour- If offensive – infection, retained cotton piece or plugs to be kept in mind.
- Amount- Scanty or absent – infection.
- Colour-Persistence red – subinvolution retained bits of conception.
- Duration- Lochia alba beyond three weeks suggestive of local lesions.
- For the first four days lochia is sterile in uterine cavity but becomes contaminated with vaginal organisms.by 5th day, vaginal organisms invade uterine cavity. presence of bacteria in lochia is considered non pathogenic in absence of clinical signs of sepsis.
Breasts and Lactation
Breasts
- The first few days both breast feeding and non-feeding breasts of women secrete colostrum, a creamy yellow precursor to milk, but the breasts remain soft and non-tender.
- Three days after delivery in response to increased prolactin level breasts become firm and tender and milk supply is initiated.
- They rapidly become distended, hard and warm because of increased flow, venous and lymphatic congestion called physiological engorgement, lasts about 24-48 hours and will resolve spontaneously, suckling by the baby stimulates ongoing milk production.

Lactation
- Lactation is under the control of numerous exocrine glands, particularly the pituitary hormones prolactin and oxytocin.
- It is influenced by the sucking process and by maternal emotions.
- Lactation, the process of breasts feeding results from interplay of hormones, instinctive reflexes and learned behaviour of the mother and new-born.
The establishment and maintenance of lactation is determined by three factors-
- The anatomical structure of the mammary gland and development of alveoli, ducts and nipples
- The initiation and maintenance of milk secretion, and
- Milk ejection or propulsion of milk from the alveoli to the nipple.
Stages of Lactation
Lactogenesis (milk initiation)- It begins during the latter part of pregnancy. Colostrum is secreted as a result of stimulation of the mammary alveolar cells by placental lactogen, a prolactin-like substance. It continues after birth as an automatic process. The continued secretion of milk is related to:
- Sufficient production of pituitary hormone prolactin.
- Maternal nutrition.
Colostrum- A yellow, premilk substance, high in protein and contains antibodies. Its production decreases gradually after childbirth and production of true milk begins. The bluish white true milk usually comes in between 3rd and 5th post-partum day. The milk at the beginning of the feeding is known as fore milk which contains less fat and flows at a faster rate than at the end of the feeding, the hind milk. Hind milk is white and contains more fat, calories and is believed to satisfy the infant and signal that the feeding should come to an end.
The last stage of human lactation is ingestion of milk by the suckling baby. The full term healthy new born baby possesses three instinctive reflexes needed for successful breast feeding-
- The rooting reflex,
- The sucking reflex, and
- The swallowing reflexes.
Maternal Breast-Feeding Reflexes
There are three major maternal reflexes involved in breast feeding which are:
- Secretion of prolactin,
- Nipple erection, and
- The let-down reflexes.
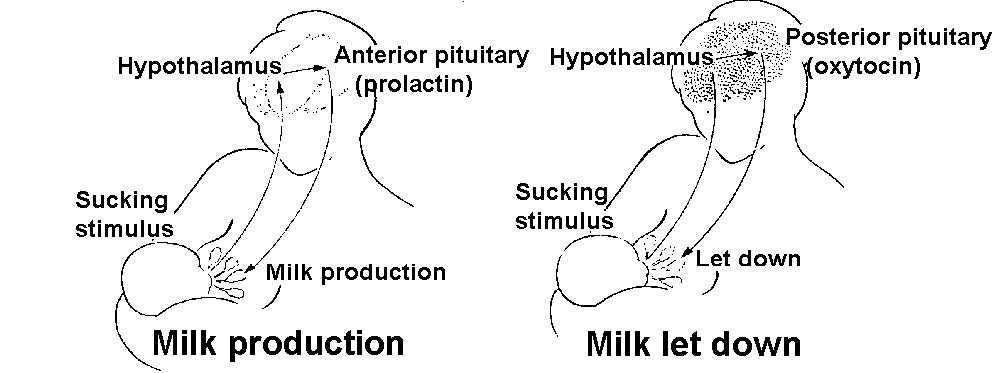
Prolactin- It is considered as the key lactogenic hormone initiating and maintaining milk secretion. Its production by the non-pituitary is mainly the result of the prolactin reflex resulting from the infant’s suckling at the breasts. The sucking stimulus provided by the baby sends a message to the hypothalamus. Hypothalamus stimulates the anterior pituitary to release prolactin, the hormone that promotes milk production in the alveolar cells of the mammary gland.
Milk production-
In the first post-partum week, the total amount of milk secreted in 24 hours is calculated to be 60 × No. of post-partum day and is expected in terms of millilitres. The milk yield on 4th day is about 60×4=240 ml and by the end of second week the milk yield is 120-180 ml per feeding.
Other System Changes-
Endocrine System-
Placental hormone-
- Insulinase causes the diabetogenic effects of pregnancy to be reversed.
- Estrogen and progesterone levels decrease markedly after expulsion of the placenta, reaching their lowest levels 1 week into the postpartum period.
- The estrogen levels in nonlactating women begin to increase by 2 weeks after birth, and higher by postpartum day 17.
Pituitary hormones and ovarian function-
- Lactating and non-lactating women differ in the time of the first ovulation.
- In women who breast feed, prolactin levels remain elevated into the sixth week after birth.
- Prolactin levels decline in nonlactating women, reaching the prepregnant range by third week.
Menstruation and Ovulation
- If the woman does not breast fed her baby, the menstruation returns by 6th week following delivery in about 40% and by 12th week in 80% of cases.
- In non-lactating mothers, ovulation may occur as early as 4 weeks and in lactating mothers about 10 weeks after delivery.
- A woman who is exclusively breastfeeding, the contraceptive protection is about 98% upto 6 months postpartum. Thus, lactation provides a natural method of contraception.
- However, ovulation may precede the first menstrual period in about one-third and it is possible for the patient to become pregnant before she menstruates following her confinement.
- Non-lactating mother should use contraceptive measures after 3 weeks and the lactating mothers after 3 months of delivery.
Urinary System-
- The bladder wall becomes oedematous and hyperaemic and often shows evidences of submucous extravasation of blood.
- Because of relative insensitivity to the raised intravesical pressure due to trauma sustained to the nerve plexus during delivery, the bladder may be overdistended without any desire to pass urine.
- Dilated ureters and renal pelvis return to normal size within 8 weeks
Cardio-Vascular System-
- Diuresis evident between second and fifth day after birth, as well as blood loss at birth, acts to reduce the added volume accumulated during pregnancy.
- Rapid reduction occurs, so that blood volume returns to its normal prepregnancy level by first or second week after birth.
- The white blood cell count sometimes reaches 30,000/L, with the increase predominantly due to granulocytes and return to normal by 4-7 days
- There is a relative lymphopenia and an absolute eosinopenia.
- Normally, during the first few postpartum days, haemoglobin concentration and haematocrit fluctuate moderately return to normal 4-5 weeks and non-pregnant levels are reached by 5-8 weeks. Blood volume: Returned to normal level by 1 week after delivery
- Cardiac Output: Remains elevated for 24 to 48 hrs postpartum and declines to nonpregnant values by 10 days.
- Heart rate changes follow this pattern
- SVR: follows inversely
- Coagulation factor return to normal in 3-4 weeks.
Gastro Intestinal System-
- Increased thirst in early puerperium due to loss of fluid during labour, lochia, diuresis and perspiration.
- Digestion and absorption begin to be active again soon after birth.
- Bowel sounds are active, but passage of stool through the bowel may be slow because of the still present effect of relaxing on the bowel.
- Bowel evacuation may be difficult because of the pain of episiotomy sutures or haemorrhoids.
Integumentary System-
- Stretch marks in women’s abdomen still appear reddened and may be even more prominent than pregnancy.
- Excessive pigment on face and neck (Chloasma) and on abdomen (Linea nigra) barely detectable in 6 weeks’ time.
- Diastasis recti (Overstretching and separation of the abdominal musculature) if present, the area will be slightly indented.
- Abdominal wall and ligaments require 6 weeks’ time to return to their former state.
Respiratory System-
After delivery with the increase in abdominal pressure, the diaphragm descents to its normal position permitting better lung expansion and ventilation but the respiratory rate does not noticeably change.
Musculo-Skeletal System-
Abdominal muscles-
Uterine ligaments remain loose and relaxed, abdominal muscles have less tone, resulting in soft, flabby abdomen. Exercise may help but restoration of the muscles may be prolonged.
Joints-
Under the influence of relaxation, the pelvis joints particularly the symphysis pubis may separate slightly during labour, causing pain and discomfort, becomes stabilized by 6-8 weeks.
postnatal exercises – Advantages
- Gives the women a sense of wellbeing ness
- Maintains good circulation, lessens possibility of venous thrombosis.
- Restores muscle tone of the abdominal wall & pelvic floor.
- Promotes for normal drainage of lochia
- Prevents hypostatic pneumonia
- Helps in emptying the bladder, bowels and uterus
- Enables her to take early care of her baby.
- Restores her body figure.
Postnatal care (Daily care)
Care of the mother
After the birth of the baby & expulsion of the placenta
1. Clean perineum & apply sterile pad
2. Make her comfortable
3. Give her a cup of tea and something light to eat (immediate)
4. Allow her to rest
5. Record vital sign
- 4 times daily for the 1st & 2nd day
- then twice daily
- if elevated as doctor ordered
6. Check for any bleeding .
Care for the baby
- Check frequently for bleeding. Give baby bath at birth and daily
- Change napkin whenever wet or soiled have mother do it.
- Take temperature twice daily or & hourly if necessary
- If the baby’s condition is good mother should be allowed to feed, as often as she wishes to do so.
- Test breast feeding and body activity of the child.
- Bring up baby’s wind often feeds.
- Check cord for bleeding and signs of infection,