National Health Policy
National Health Policy
Health
Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.

National
National is used to describe something that belongs to or is typical of a particular country or nation.
POLICY
Policy is a system, which provides the logical framework and rationality of decision making for the achievements of intended objectives.
HEALTH POLICY
Health policy of a Nation is its strategy for controlling and optimizing the social uses of its health knowledge and health resources.
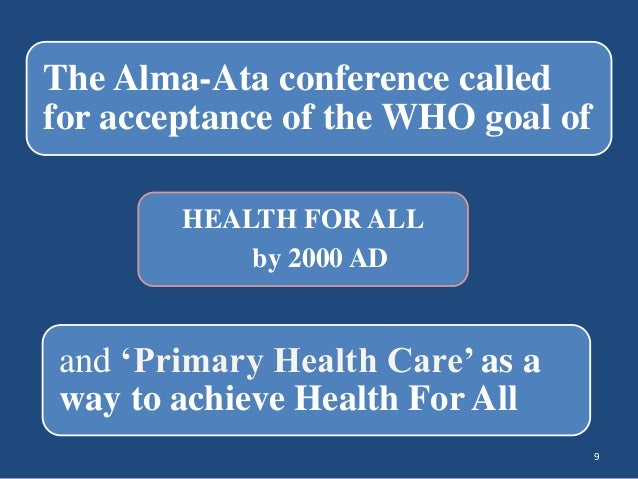
The Joint WHO – UNICEF international conference in 1978 at Alma-Ata (USSR) declared that
NATIONAL HEALTH POLICY (1983)
To attain the objectives “Health for all by 2000 AD”, the Union Ministry of Health and Welfare formulated National Health Policy 1983.
NATIONAL HEALTH POLICY- 1983
- India had its first National health policy in 1983 i.e. 36 years after independence.
- In the circumstances then prevailing, this policy provided the initiatives like-
- Comprehensive health care linking with extension and health education.
- Intermediation by health volunteers
- Decentralization to reduce burden of high level referral system
- To make government facility limited to eligible poor, by private investment for patients who can pay.
- NATIONAL HEALTH POLICY 1983 suggested the necessity of complete integration of all plans for human development with socio economic development. Health related sectors like Pharmaceuticals, Agriculture, Rural development, education, Social Welfare, Housing, Water supply and conservation of environment were integrated for joint venture.
- National health policy 1983 stressed the need for providing primary health care with special emphasis on prevention , promotion and rehabilitation aspects.
- Its emphasis is on team approach, ban on private practice by health professionals and use of our large stock of health manpower from alternative system of medicine like Ayurveda, Unani, Sidda, Homoeopathy, Yoga and Naturopathy.
- It suggested Planned time bound attention to the following
- Nutrition, prevention of food adulteration.
- Maintenance of quality of drug
- Water supply and sanitation
- Environmental protection
- Immunisation Programme
- Maternal and Child Health Services
- School Health Programme
- Occupational Health
- It also suggested the need for meeting National requirements of life saving drugs and vaccines by quality control, economic packages practice, reduction in unit cost of medicine and well considered health insurance schemes to allow community to share the cost of the services, in keeping with the paying capacity.
KEY ELEMENTS OF NATIONAL HEALTH POLICY 1983
- Creation of greater awareness of health problems in the community and means to solve the problems by the community.
- Supply of safe drinking water and basic sanitation using technologies that people can afford.
- Reduction of existing imbalance in health services by concentrating more on the rural health infrastructure.
- Establishing of dynamic health management information system to support health planning and health program implementation.
- Provision of legislative support to health protection and promotion.
- Concerned actions to combat wide spread malnutrition.
- Research in alternative method of health care delivery and low cost health technologies.
- Greater co-ordination of different system of medicine.
NATIONAL HEALTH POLICY 1983 GOALS SUGGESTED/ ACHIEVED
| INDICATOR | GOAL BY 2000 | ACHIEVED BY 2000 |
| INFANT MORTALITY RATE (IMR) | 60 | 70 |
| PERI NATAL MORTALITY RATE (PNMR) | 33 | 46 |
| CRUDE DEATH RATE (CDR) | 9 | 8.7 |
| MATERNAL MORTALITY RATE (MMR) | 2 | 4 |
| UNDER FIVE MORTALITY RATE (UFMR) | 10 | 9.4 |
| LIFE EXPENTANCY BIRTH MALE(yrs.) FEMALE(yrs.) |
64 64 |
62.4 63.4 |
| LOW BIRTH WEIGHT % | 10% | 20% |
| CRUDE BIRTH RATE | 21 | 26.1 |
| COUPLE PROTECTION RATE | 60% | 46.2% |
| NET REPRODUCTION RATE | 1 | 1.45 |
| GROWTH RATE | 1.2 | 1.93 |
| FAMILY SIZE | 2.3 | 3.1 |
| ANTE NATAL CARE (ANC) | 100% | 67.2% With ANC still less with full ANC |
| TT PREGNANT | 100% | 83 |
| DPT | 85 | 87 |
| OPV | 85 | 92 |
| BCG | 85 | 82 |
FACTORS INTERFERING WITH THE PROGRESS TOWARDS HEALTH FOR ALL:-
- Insufficient political commitment to the implementation on Health for All.
- Failure to achieve equity in access to all primary health care elements.
- The continuing low status of women.
- Slow socio-economic development.
- Difficulty in achieving intersectoral action for health.
- Unbalanced distribution of and weak support for human resources.
- Widespread inadequacy of health promotion activities.
- Weak health information system and no baseline data.
- Pollution, poor food, safety, and lack of water supply and sanitation.
- Rapid demographic and epidemiological changes.
- Inappropriate use of and allocation of resources, high-cost technology.
- Natural and man-made disasters.
NATIONAL HEALTH POLICY-2002
- A revised health policy for achieving better health care and unmet goals has been brought out by government of India- National Health Policy 2002.
- According to this revised policy, government and health professionals are obligated to render good health care to the society.
- Optimizing the use of health service to a large group rather than a small group is a foreseen event by the NHP 2002.
- Inclusion of social policies adds to the credit of the revised NHP 2002.
- NHP2002 has set out a new policy framework for the acceleration of Public Health goals in the socioeconomic circumstances currently prevailing in the country.
Goals to be Achieved by 2000-2015
|
Eradicate Polio and Yaws |
2005 |
| Eliminate Leprosy | 2005 |
| Establish an integrated system of surveillance | 2005 |
| Increase share of central grants to Constitute at least 35% of total Health spending | 2005 |
| Achieve zero level growth of HIV/AIDS | 2007 |
| Eliminate Kala-Azar | 2010 |
| Reduce mortality by 50% On account of TB, Malaria | 2010 |
| Other vector born and water born Prevalence of blindness to 0.5% | 2010 |
| Reduce IMR to 30/1000 and MMR to 100/lakh | 2010 |
| Improve nutrition and reduce LBW Babies from 30% to 10% | 2010 |
| Increase the utilization of Public Health Facilities from current >20 to <75% | 2010 |
| Eliminate Lymphatic Filariasis | 2015 |
National Health Policy 2002
Objectives-
- Achieving an Acceptable standard of good health of Indian Population.
- Decentralizing public health system by upgrading infrastructure in existing institutions.
- Ensuring a more equitable access to health service across the social and geographical expanse of India.
- Enhancing the contribution of private sector in providing health service for people who can afford to pay.
- Emphasizing rational use of drugs.
- Increasing access to tried systems of Traditional Medicine
NATIONAL HEALTH POLICY 2017
Goal
Attainment of highest possible level of health and well being for all at all age groups. through a preventive and promotive health care orientation in all developmental policies, and universal access to good quality health care services without anyone having to face financial hardship as a consequence.
Key policy principles
- Professionalism. integrity and ethics
- Equity
- Affordability
- Universality
- Patient centred and quality care
- Accountability
- Inclusive partnership
- Pluralism(AYUSH)
- Decentralization
- Dynamism and adaptiveness
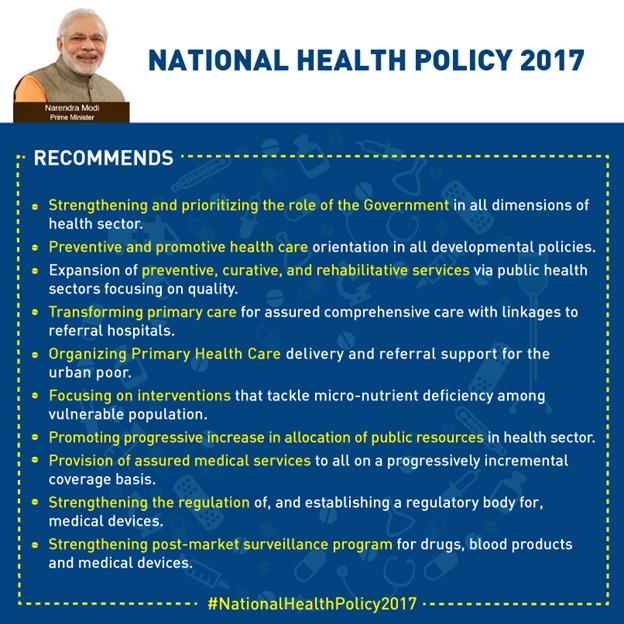
Preventive and Promotive Health
The policy identifies coordinated action on seven priority areas for improving the environment for health-
- The Swachh Bharat Abhiyan
- Balanced, healthy diets and regular exercises.
- Addressing tobacco, alcohol and substance abuse
- Yatri Suraksha – preventing deaths due to rail and road traffic accidents
- Nirbhaya Nari –action against gender violence
- Reduced stress and improved safety in the work place
- Reducing indoor and outdoor air pollution
CONCLUSION
While the public health initiatives over the years have contributed significantly to the improvement of the health indicators, it is to be acknowledged that public health indicators/ disease burden statistics are the outcome of several complementary initiatives under the wider umbrella of the developmental sector, covering rural development, agriculture, food production, sanitation, drinking water supply, education etc.
- Despite the impressive public health gains, the morbidity and mortality levels in the country are still unacceptably high as compared to the developed countries.
- Further dedicated efforts are required to achieve goal of ‘Health for All’ in 21st century’.
- NHP 2002 will provide an impetus for achieving an acceptable standard of good health of people of India.