Sterilisation and Disinfection
Sterilisation
It is a process by which an article, surface or medium is made free of all microorganisms either in the vegetative or spore form.
Disinfection
It means the destruction of all pathogens or organisms capable of producing infections but not necessarily
spores. All organisms may not be killed but the number is reduced to a level that is no longer harmful to health.
Less lethal than sterilization. Destroys most recognized pathogenic organisms but not necessarily all microbes (e.g. Spores)
Purpose-prevent transmission of certain microorganisms with objects, hands or skin and prevent spreading the infection.
Physical or chemical methods.
Uses of Sterilisation/Disinfection
- Sterilisation of materials, instruments used in surgical and diagnostic procedures.
- For media and reagents used in the microbiology laboratory.
METHODS OF STERILISATION
A. Physical Methods
1. Sunlight
2. Heat:
- Dry heat
- Moist heat
3. Ozone
4. Filtration
5. Radiation
B. Chemical Methods
- Alcohols
- Aldehydes
- Phenols
- Halogens
- Oxidising agents
- Surface active agents
- Dyes
- Gases
A. Physical Methods
1. Sunlight
Sunlight has an active germicidal effect due to its conten of ultraviolet rays. It is a natural method of sterilisation
in cases of water in tanks, rivers and lakes
2. Heat
Heat is the most reliable and commonly employed method of sterilisation. Two types of heat are used, dry
heat and moist heat.
Principle
- Dry heat kills the organisms by denaturation of bacterial protein, oxidative damage and by the toxic effect of elevated levels of electrolytes
- Moist heat kills the microorganisms by denaturation and coagulation of proteins
Dry heat sterilisation
The following procedures are used for sterilisation by dry heat.
- Red heat
- Flaming
- Incineration
- Hot air oven
1. Red heat
Inoculating wires or loops, tips of forceps and needles are held in the flame of a Bunsen burner till they become red hot.
2. Flaming
Glass slides, scalpels and mouths of culture tubes are passed through bunsen flame without allowing them to
become red hot.
3. Incineration
By this method, infective material is reduced to ashes by burning. Instrument named incinerator may be used for this purpose. Soiled dressings, animal carcasses, bedding and pathological materials are dealt with this method. It is also one of the methods for treatment of biomedical waste and disposal.
4. Hot Air Oven
It is the most widely used method of sterilisation by dry heat. The oven is electrically heated and is fitted With a fan to ensure adequate and even distribution of hot air in the chamber. It is also fitted with a thermostat that maintains the chamber air at a chosen temperature
Temperature and time
160°C for two hours (holding time) is required for sterilisation.
Uses-
It is used for sterlisation of
- Glass-wares like glass syrings, petridishes, flasks, pipettes and test tubes.
- Surgical instruments like scalpels scissor, forceps etc.
Precautions
- It should not be overloaded.
- The material should be arranged in a manner which allows free circulation of air.
- Material to be sterilised should be perfectly dry.
- Test tubes, flasks etc. should be fitted with cotton plugs.
- Petridishes and pipettes should be wrapped in craft paper.
- Rubber materials (except silicone rubber) or any inflammable material should not be kept inside the Oven.
- The oven must be allowed to cool for two hours before opening the doors, since the glasswares may crack by sudden cooling.
Sterilisation control
- The spores of nontoxigenic strain of Clostridium tetani are kept inside the oven. These spores should be destroyed if the sterilisation is proper.
- Thermocouples may also be used.
- Browne's tube with green spot is available. After proper sterilisation a green colour is produced (after two hours at 160°C).
Moist heat sterilisation
This method of sterilisation may be used at different temperatures as follows.
- At a temperature below 100°C
- At a temperature of 100°C
- At a temperature above 100°C
(i) At a Temperature below 100°C
a. Pasteurisation of milk -Two types of method, holder method, (63°C for 30 minutes) and flash method (72°C for 20 seconds followed by cooling quickly to 13°C or lower) are used.
b. Inspissation- Some serum or egg media, such as Lowenstein-Jensen's and Loeffler's serum, are rendered sterile by heating at 80-85°C temperature
for half an hour daily on three consecutive days. This process of sterilisation is called inspissation. The instrument used is called inspissator.
c. Low temperature steam formaldehyde (LTSF) sterilisation -Items the temperature of 100°C may be sterilised by a method known as low temperature steam formaldehyde (LTSF) sterilisation. method steam at subatmospheric pressure at the temperature of 75°C with formaldehyde vapour is used. Geobacillus stearothermophilus has been used as biological control to test the efficacy of LTSF sterilisers.
ii) At a Temperature of 100°C
a. Boiling-Boiling for 10 to 30 minutes may kill most of the vegetative forms but many spores withstand boiling for a considerable time. When
better methods are not available, boiling may be used for glass syringes and rubber stoppers. It is not recommended for the sterilisation of
instruments used for surgical procedures.
b. Tyndallisation or Intermittent sterilisation-
Steam at 100°C for 20 minutes on three successive days is used, This is known s tyndallisation or intermittent sterilisation, The principle is that the first exposure kills all the vegetative forms, in the intervals between the heatings the remaining spores germinate into vegetative forms which are kiled on subequent heating, it is used for sterilisation of egg, serum or sugar containing media which are damaged at higher temperature of autocave
At a Temperature above 100°C
(under pressure)
Water boils when its vapour premure equals that of the surrounding atmosphere. When the atmospheric prevsure is raised then the boiling temperature is also raised. As normal pressure water boils at 100°C but when pressure inside a closed vessel increases, the temperature at which
water boils also increases. This principle has been applied in autoclave and pressure cooker
Autoclave
Principle
Steam above 100°C or saturated steam has a better killing power than dry heat, Bacteria are more susceptible to moist heat as bacterial protein coagulates rapidly Saturated steam can penetrate porous material easily When steam comes into contact with a cooler surface it condenses to water and liberates its latent heat to that surface, for example, 1600 ml of steam at 100°C and at atmospheric presure condenses into one ml of water
at 100°C and releases 518 calories of heat. The large reduction in volume sucks in more steam to the same site and the proces6 continues till the temperature of the article is raised to that of steam, The condensed water produces moist conditions for killing the microbes present.
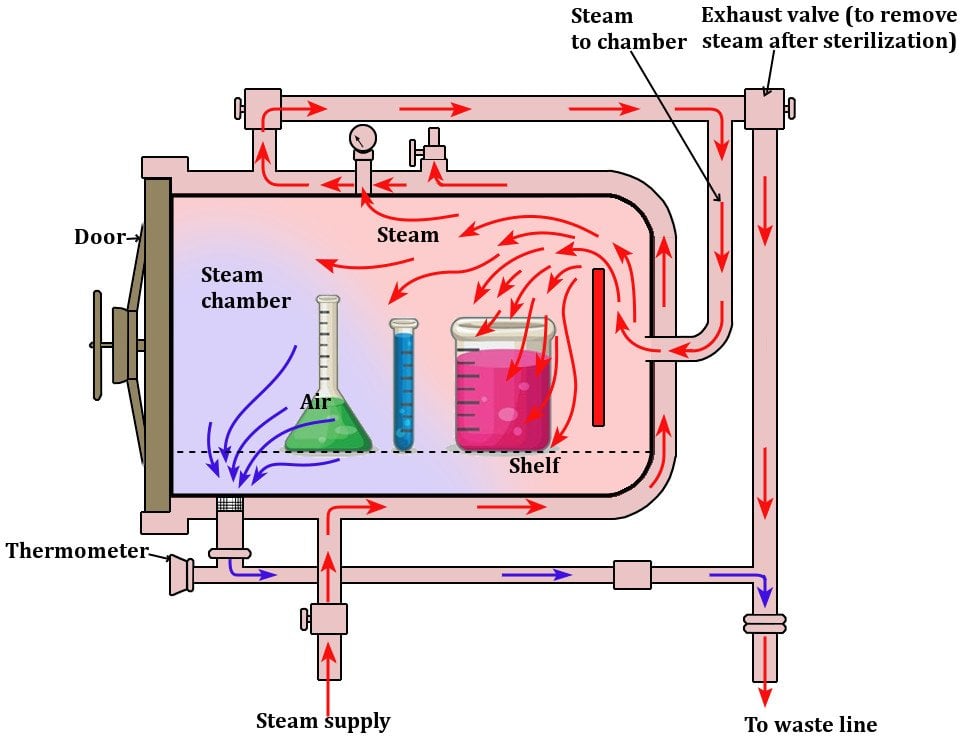
Components of autoclave
Autoclave is a modified pressure cooker or boiler. It consists of a vertical or horizontal cylinder of gunmetal or stainless steel in a supporting iron case. The lid is fastened by screw clamps and rendered air tight by an asbestos washer. T'he lid bears a discharge tap for air and steam, a pressure gauge and a safety valve. Heating is generally done by electricity. The steam circulates within the jacket and is supplied under high pressure to the
inner chamber where materials are kept for sterilisation.
Sterilisation conditions
Temperature-121°C
Chamber pressure-15 pounds (lbs) per square inch
Holding time-15 minutes
These conditions are generally used, however, sterilisation can also be done at higher temperatures, at 126°C (20 lbs/square inch) for 10 minutes or at 133°C (30 lbs/square inch) for 3 minutes.
Uses
- To sterilise culture media, rubber material, gowns, dressing, gloves etc.
- It is particularly useful for materials which cannot withstand the higher temperature of hot air oven
- For all glass syringes, hot air oven is a better sterilising method.
Precautions
- The air must be allowed to escape from the chamber as temperature of air-steam mixture is lower than that of pure steam.
- Materials should be arranged in such a manner as to ensure free circulation of steam inside the chamber.
Sterilisation control
1. Thermocouple--It is to record the temperature directly by a potentiometer.
2. Bacterial spores- Spores of stearothermophilus are used as the test organism. The spores of this organism are killed in 12 minutes at 121°C. An envelope containing a filter paper strip impregnated with 100 spores is placed inside the autoclave during sterilisation. Spores are destroyed
if sterilising conditions of autoclave are proper.
3. Chemnical indicators -Browne's tube contains red solution which turns green, when exposed to temperature of 121°C for 15 minutes in autoclave.
4. Autoclave tapes
3. Ozone
Low temperature sterilisation by ozone
Ozone steriliser uses oxygen, water and electricity to produce ozone within the steriliser and provide sterilisation without producing toxic chemicals. It runs at lower temperature, i.e., 25°C-35°C. In this device, Oxygen molecules (O2) are separated into atomic oxygen (0) in the preence of intense electrical field. These atomic Oxygen (O) combines with other oxygen molecules (02) to form ozone (O3). The ozone provides a steriligy assurance of 10-6 in approximately 4 hours.
4. Filtration
This method of sterilisation is useful for substances which get damaged by heat process e.g. sera, sugars, antibiotic solutions etc.
Uses of filtration
- To sterilise sera, sugars and antibiotic solutions.
- Separation of toxins and bacteriophages from bacteria.
- Sterilisation of hydatid fluid.
Types of filters
1. Earthenware candles -These filters are usually made in the form of hollow candles. The liquid to be filtered is passed through the candle. They are
available in different grades of porosity.
2. Asbestos disc filters (Seitz filter)-These are no longer used due to carcinogenie property of asbestos.
3. Sintered glass filters-These are prepared by fusing finely powdered glass particles. These are available in different pore sizes.
4. Membrane filters-Membrane filters are made up of cellulose esters. Nitrocellulose (Millipore) membrane filters are widely used. Membrane filters
are available in pore sizes of 0.015 to 12 um.
5. Air filters-These filters are used to deliver clean bacteria-free air to a cubicle or a room. High efficiency particulate air (iEPA) hlters are used in air filtration in laminar air flow system in microbiology laboratories. HEPA filters can remove particles of 0.3 um or larger.
5. Radiations
Two types of radiations are used for sterilisation: ionising and non-ionising.
1. lonising radiations-lonising radiations include gamma rays, X-rays and cosmic rays. They are highly lethal to all cells including bacteria. They damage DNA by various mechanisms. Gamma radiations are commercially used for sterilisation of disposable items such as plastic syringes, swabs,
culture plates, cannulas, catheters etc. This method is also known as cold sterilisation because there is no appreciable increase in temperature.
2. Non-ionising radiations-These include infrared and ultraviolet (UV) radiations. Infrared is used for rapid mass sterilisation of syringes and catheters. Ultraviolet radiatioon has marked bactericidal activity. It acts by denaturation of bacterial protein and interference with DNA replication. UV
radiation is used for disinfecting enclosed areas such as bacteriological laboratory, inoculation hoods, laminar flow and operation theatres