Bed Sores
Bed Sores-Decubitus ulcer or bedsore or pressure ulcer is an ulceration sloughed area of tissue resulting from pressure, slowing of circulation and causing death of cells.
DEFINITION-
- A Pressure Ulcer or Pressure Sore or Decubitus Ulcer or Bedsore is localized injury to the skin and other underlying tissue, usually over a body prominence, as a result of prolonged unrelieved pressure.
- Decubitus ulcer is an ulcer occurring on the skin of any bed ridden patient particularly over the Bony prominences or skin folds where the surfaces rub against each other.
Purpose:-
- To enhance circulation.
- To promote healing.
- Prevent from infection.
- To treat bed sore.
- Prevent further damage.
Cause/Risk Factors
- Friction
- Shear
- Moisture
- Edema
- Obesity
- Impaired Sensory Perception
- Impaired Physical Mobility
- Altered Level Of Consciousness
- Fecal And Urinary Incontinence
- Malnutrition
- Dehydration
- Excessive Body Heat
- Advanced Age
- .Chronic Medical Conditions- Diabetes, Cardiovascular Diseases.
Sign and Symptoms/Clinical Manifestation:-
1. Early symptoms are:-
- Tenderness
- Redness
- Discomfort
- Stinging pain
- Local edema
2. Late symptoms are:-
- Area becomes blue, purple or mottled
- Gangrene develop in late stage
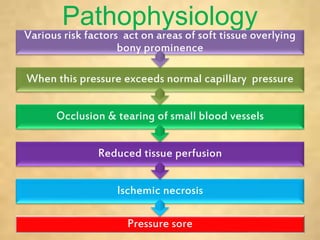
Pathophysiology
Pressure sore Ischemic necrosis Reduced tissue perfusion Occlusion & tearing of small blood vessels When this pressure exceeds normal capillary pressure Various risk factors act on areas of soft tissue overlying bony prominence.
Common Sites:-
1. When the patient is in supine position-
- Back of the head (occiput)
- Scapula
- Nape of the neck
- Sacral region most common area
- Elbows and heels.
2. In side lying position, pressure point are-
- Ear
- Acromion process of the shoulder
- Ribs, iliac crest
- Greater trochanter of the hips
- Medial and lateral condyles of knee.
- Malleolus of the ankle joint.
3. In prone position, pressure points are-
- Back of the ears and check.
- Acromion process, knee and toes
Stages / Classification Of Bedsores
- Staging systems for pressure ulcers are based on the depth of tissue destroyed.
- Based on the depth there are four stages of bedsores
- Stage I
- Stage II
- Stage III
- Stage IV
1. Stage I: Nonblanchable Redness of Intact Skin
- Intact skin presents with nonblanchable erythema of a localized area usually over a bony prominence.
- Discoloration of the skin, warmth, edema or pain may also be present
- Stage I indicates “at-risk” persons.
- Involves only the epidermal layer of skin.

2. Stage II: Partial-thickness Skin Loss Or Blister.
- A partial thickness loss of dermis presents as a shallow open ulcer with a red-pink wound bed without slough
- Stage II is damage to the epidermis and the dermis. In this stage, the ulcer may be referred to as a blister or abrasion.

3. Stage III: Full-thickness Skin Loss (Fat Visible).
- A stage III ulcer is a full-thickness tissue loss. Subcutaneous fat may be visible; but bone, tendon, or muscle is not exposed.
- Epidermis, dermis and subcutaneous tissues involved
- Subcutaneous layer has a relatively poor blood supply. So its difficult to heal.
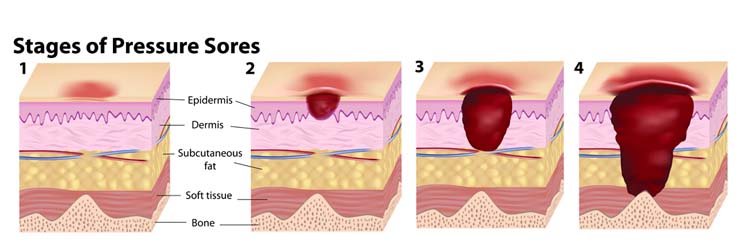
4. Stage IV: Full-thickness Tissue Loss
- Full thickness tissue loss
- Muscle and bone visible
- Epidermis, dermis, subcutaneous tissue, bone, tendon, muscle damage
Complications
- Cellulitis
- Bone and joint infections
- Sepsis
- Cancer
Prevention
- Bedsores are easier to prevent than to treat. Although wounds can develop in spite of the most scrupulous care, it's possible to prevent them in many cases.
1. Position changes
- Changing position frequently and consistently is crucial to preventing bedsores. Experts advise shifting position about every 15 minutes that you're in a wheelchair and at least once every two hours, even during the night, if you spend most of your time in bed.
2. Skin inspection
- Daily skin inspections for pressure sores are an integral part of prevention.
3. Nutrition
- A healthy diet is important in preventing skin breakdown and in aiding wound healing Adequate hydration to maintain the skin integrity.
4. Lifestyle changes
- Quitting smoking Exercise
- Daily exercise improves circulation
5. Use pressure-
- Relieving devices such as air mattress, water mattress.
Treatment
1. Changing positions often.
Carefully follow the schedule for turning and repositioning
- Approximately every 15 minutes if in a wheelchair and at least once every two hours when in bed.
- If unable to change position on own, a family member or other caregiver must be able to help.
2. Using support surfaces.
- These are special cushions, pads, mattresses and beds that relieve pressure on an existing sore and help protect vulnerable areas from further breakdown.
3. Cleaning.
- It's essential to keep wounds clean to prevent infection. A stage I wound can be gently washed with water and mild soap, but open sores should be cleaned with a saltwater (saline) solution each time the dressing is changed.
4. Controlling incontinence
5. Removal of damaged tissue (debridement). To heal properly, wounds need to be free of damaged, dead or infected tissue.
6. Dressings.-This should occur at the time of soiling and at routine intervals. The frequency of skin cleansing should be individualized according to patient needs and preference
7. Pressure Point Care
- It includes the relieving of pressure from highly vulnerable areas with the help of comfort devices or range of motion exercises.
- Back care is a traditional practice that is done from many years as it promotes circulation, relieve the pressure, relieve the pain or muscle tension and the main one is to prevent the pressure ulcers.
8. Oral antibiotics. To prevent infection.
9. Healthy diet.
- Assess the patient's need to eat independently, ask the patient for his/her choice of food also.
- Check mainly the albumin and total protein count of the patient.
- Take high protein diet such as egg, milk and milk products.
- Take vitamin and other supplements to maintain skin integrity.
- Provide and encourage adequate daily fluid intake for hydration maintenance.
10. Educating the caregiver
Surgical Repair
- Tissue flap.
- Plastic surgery may be required to replace the tissue.
Role Of Nurse In Prevention & Management Of Bed Sores \
The nurse should be continuingly assessing the client who are at risk for pressure ulcer development
1. Assess the client for-
- The predisposing factors for bed sore Development.
- Skin condition at least twice a day.
- Inspect each pressure sites.
- Palpate the skin for increased warmth.
- Inspect for dry skin, moist skin, breaks in skin
- Evaluate level of mobility.
- Evaluate circulatory status (eg. Peripheral pulses, edema).
- Assess neurovascular status.
- Determine presence of incontinence
- Evaluate nutritional and hydration status.
- Note present health problems.
2. Interventions for a patient with Decreased sensory perception
- Assess pressure points for signs of bed sore development.
- Provide pressure-redistribution surface.
3. Interventions for a patient with incontinence
- Assess need for incontinence management.
- Following each incontinent episode, clean area and dry thoroughly.
- Protect skin with moisture-barrier ointment.
4. Interventions to avoid Friction and shear
- Reposition patient using draw sheet and lifting off surface.
- Use proper positioning technique.
- Avoid dragging the patient in bed
- Use comfort devices appropriately.
5. Interventions for a patient with Decreased activity/ mobility
- Establish individualized turning schedule.
- Change position at least once in two hours and more frequently for the high risk individuals.
6. Interventions for a patient with Poor Nutrition
- Provide adequate nutritional and fluid intake
- Assist with intake as necessary.
- Consult dietitian for nutritional evaluation
- Evaluate the ulcer progress every 4-6 days.
- Assist the physician or surgeon in debridement
- Educate the patient and family regarding the risk factors and prevention of bed sores.