Angina Pectoris
Introduction
The heart requires a balance between oxygen supply and oxygen demand in order to function properly. Any disorder that reduces the lumen of one of the coronary arteries may cause a decrease in blood flow and oxygen delivery to the area of the myocardium supplied by that vessel and lead to acute coronary syndromes of angina, acute myocardial infarction and sudden cardiac death.
Angina Pectoris
- A disease marked by brief sudden attacks of chest pain or discomfort caused by deficient oxygenation of the heart muscles usually due to impaired blood flow to the heart.
- Angina pectoris or chest pain is a clinical syndrome produced by insufficient Coronary blood flow leading to transient myocardial ischemia.
- Angina pectoris is chest pain resulting from myocardial ischemia (inadequate blood supply to the myocardium).
Risk Factors for Angina-
Myocardial Ishemia which occurs when there is 75 percent or more block in a coronary artery due to arthroscleosis, forcing flow of blood through the stenosis vessel causing coronary artery spasm which is transient and reversible.
- Advanced age
- Coronary artery disease
- Increase serum glucose levels (Diabetes)
- Increase serum lipoprotein levels
- Obesity
- Hypertension
- Smoking
- Decrease oxygen supply to Myometrium like -COPD,Anemia, Hypoxemia etc.
- Type A personality
Initiating Factors –
- Cold weather
- Heavy meals
- Physical exertion
- Hypoglycemia
- Strong Emotions
- Stimulated drug abuse. e.g.-cocaine
Types of Angina-
1. Stable angina- Chest pain occurring intermittently over a long period within the same pattern of onset, during and intensity of symptom.
- Effort-induced pain from physical activity or emotional stress.
- Relieved by rest
- Predictable and reproducible
2. Unstable angina-This is unpredictable. A stable angina may develop into unstable angina. The angina will be occurring with increasing frequency minimal or no exercise, during sleep or even at total rest.
- Pain occurs with increasing frequency
- Has decrease response to therapy.
- May signal an oncoming MI
3. Prinzmetal's angina or Variant Angina-It occurs at rest, usually in response to spasm of a coronary artery spasm may be due to increased myocardial oxygen demand, or increase in levels of substances like histamine, angiotensin, epinephrine, prostaglandin.
- Pain due to coronary artery spasm.
- Pain may occur at certain times of the day, but is note stress induced.
4. Nocturnal Angina- Angina occurs in the night, but not necessarily when the person is in recumbent position or during sleep.
5. Decubitus Angina-Angina occurs only while the person is lying down and is usually relieved by standing or sitting.
Symptoms of Angina-
- Sever chest discomfort
- Chest pain- May be mid-anterior chest, substernal, epigastric region, radiation to neck, back, arms, fingers
- Pain Onset-Angina attack can develop quickly or slowly
- Location-80-90% of client experience the pain as retrosternal or slightly to the left of the sternum.
- Radiation -Radiate to the left shoulder and upper arm.
- Duration-usually last a short time less then 5 minutes
- Sensation-Squeezing,burning,pressing
- Severity-Mild to moderate
- Relieving -Nitroglycerine or Rest
- Sweating
- Dizziness
- Dyspnea
Onset and Duration-Gradual or sudden onset, usually duration of less than 15 minutes, relief from nitroglycerine.
Diagnosis-
- History and physical examination
- X-ray chest
- Echocardiography, ECG
- Lipid studies, enzyme series
- Exercise ECG, Holter ECG
- Nuclear Studies
- PET-A positron emission tomography (PET) scan of the heart is an imaging test that uses specialized dye to allow your doctor to view problems with your heart.
- Coronary Angiography
- Cardiac catheterization and angiogram
Treatment-
- Treatment for coronary artery disease usually involves lifestyle changes and, if necessary, drugs and certain medical procedures.
- Lifestyle changes
- Making a commitment to the following healthy lifestyle changes can go a long way toward promoting healthier arteries:
- Quit smoking.
- Eat healthy foods.
- Exercise regularly.
- Lose excess weight.
- Reduce stress.
Drugs-
Various drugs can be used to treat coronary artery disease, including:
- Cholesterol-modifying medications- By decreasing the amount of cholesterol in the blood, especially low-density lipoprotein (LDL, or the "bad") cholesterol, these drugs decrease the primary material that deposits on the coronary arteries. Your doctor can choose from a range of medications, including statins, niacin, fibrates and bile acid sequestrants.
- Aspirin- Your doctor may recommend taking a daily aspirin or other blood thinner. This can reduce the tendency of your blood to clot, which may help prevent obstruction of your coronary arteries.If you've had a heart attack, aspirin can help prevent future attacks. There are some cases where aspirin isn't appropriate, such as if you have a bleeding disorder or you're already taking another blood thinner, so ask your doctor before starting to take aspirin.
- Beta blockers- These drugs slow your heart rate and decrease your blood pressure, which decreases your heart's demand for oxygen. If you've had a heart attack, beta blockers reduce the risk of future attacks.
- Calcium channel blockers-These drugs may be used with beta blockers if beta blockers alone aren't effective or instead of beta blockers if you're not able to take them. These drugs can help improve symptoms of chest pain.
- Ranolazine- This medication may help people with chest pain (angina). It may be prescribed with a beta blocker or instead of a beta blocker if you can't take it.
- Nitroglycerin-Nitroglycerin tablets, sprays and patches can control chest pain by temporarily dilating your coronary arteries and reducing your heart's demand for blood.
- Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs)-These similar drugs decrease blood pressure and may help prevent progression of coronary artery disease.
Procedures to restore and improve blood flow
- Coronary artery stent
- Coronary bypass surgery
Special Therapeutic Procedure-
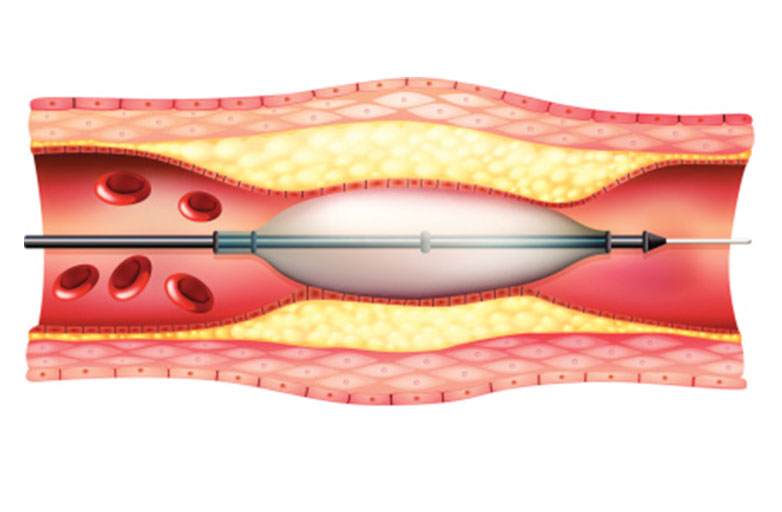
Percutaneous transluminal coronary angioplasty.stent placement, atherectomy, lazer angioplasty and coronary artery bypass graft.
- Percutaneous transluminal coronary angioplasty (PTCA)-A specially designed balloon tipped catheter is introduced into the coronary artery to open the narrowed portion of the coronary artery. The catheter is passed through the femoral artery into the aorta and then into the affected coronary artery. Then the balloon is inflated and the atherosclerotic plaque is compressed against the arterial wall resulting in opening of the blocked lumen of the vessel.
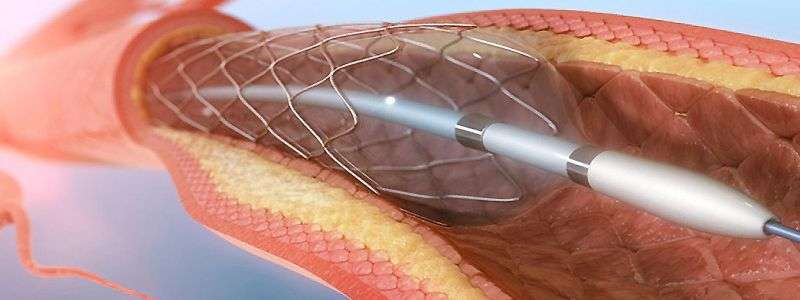
- Stent placement-Stents are expandable mesh-like structure designed to maintain vessel patency by compressing the arterial wall and resisting abrupt closure following PTCA. They are threaded on the PTCA catheter.
.jpg)
- Atherectomy- A special device is used to shear off the atheromatus plague. this device is positioned is such a way that the dislodged plaque is sucked into the catheter.
- Lazer Angioplasty-A catheter is introduced through a peripheral artery into the diseased coronary artery. A small leaser on the tip of catheter vaporizes the plaqued areas of the artery, facilitating the blood flow.
Lifestyle and home remedies
- Lifestyle changes can help you prevent or slow the progression of coronary artery disease.
- Stop smoking. Smoking is a major risk factor for coronary artery disease. Nicotine constricts blood vessels and forces your heart to work harder, and carbon monoxide reduces oxygen in your blood and damages the lining of your blood vessels. If you smoke, quitting is one of the best ways to reduce your risk of a heart attack.
- Control your blood pressure. Ask your doctor for a blood pressure measurement at least every two years. He or she may recommend more-frequent measurements if your blood pressure is higher than normal or you have a history of heart disease. Optimal blood pressure is less than 120 systolic and 80 diastolic, as measured in millimeters of mercury (mm Hg).
- Check your cholesterol. Ask your doctor for a baseline cholesterol test when you're in your 20s and at least every five years. Most people should aim for an LDL cholesterol level below 130 milligrams per deciliter (mg/dL), or 3.4 millimoles per liter (mmol/L) If you have other risk factors for heart disease, your target LDL cholesterol may be below 100 mg/dL (2.6 mmol/L).
- Keep diabetes under controlI. f you have diabetes, tight blood sugar management can help reduce the risk of heart disease. . Exercise helps you achieve and maintain a healthy weight and control diabetes, elevated cholesterol and high blood pressure — all risk factors for coronary artery disease. For example, try walking for about 30 minutes on most or all days of the week.
- Participate in cardiac rehabilitation. If you've had surgery, your doctor may suggest you participate in cardiac rehabilitation — a program of education, counseling and exercise training that's designed to help improve your health.
- Eat healthy foods. A heart-healthy diet, such as the Mediterranean diet, that emphasizes plant-based foods, such as fruits, vegetables, whole grains, legumes and nuts — and is low in saturated fat, cholesterol and sodium — can help you control your weight, blood pressure and cholesterol. Eating one or two servings of fish a week also is beneficial.
- Avoid saturated fat and strans fat, excess salt, and excess sugar. If you drink alcohol, drink it in moderation — this means up to one drink a day for women of all ages and men older than age 65, and up to two drinks a day for men age 65 and younger. One drink equals 12 ounces of beer, 5 ounces of wine or 1.5 ounces of 80-proof liquor.
- Maintain a healthy weight. Being overweight increases your risk of coronary artery disease. Losing even just a small percentage of your current weight can help reduce risk factors for coronary artery disease.
- Manage stress. Reduce stress as much as possible. Practice healthy techniques for managing stress, such as muscle relaxation and deep breathing.
- Get your flu shot. Get your flu (influenza) vaccine each year to reduce your risk of having influenza. In addition to healthy lifestyle changes, remember the importance of regular medical checkups. Some of the main risk factors for coronary artery disease — high `cholesterol, high blood pressure and diabetes — have no symptoms in the early stages. Early detection and treatment can set the stage for a lifetime of better heart health.
Alternative medicine
- Omega-3 fatty acids are a type of unsaturated fatty acid that's thought to reduce inflammation throughout the body, a contributing factor to coronary artery disease. However, some research has not found them to be beneficial. More research is needed. Fish and fish oil.
- Fish and fish oil are the most effective sources of omega-3 fatty acids. Fatty fish — such as salmon, herring and light canned tuna — contain the most omega-3 fatty acids and, therefore, the most benefit. Fish oil supplements may offer benefit, but the evidence is strongest for eating fish.
- Flax and flaxseed oil. Flax and flaxseed oil also contain beneficial omega-3 fatty acids, though studies have not found these sources to be as effective as fish. The shells on raw flaxseeds also contain soluble fiber, which can help with constipation. More research is needed to determine if flaxseed can help lower blood cholesterol.
- Other dietary sources of omega-3 fatty acids. Other dietary sources of omega-3 fatty acids include canola oil, soybeans and soybean oil. These foods contain smaller amounts of omega-3 fatty acids than do fish and fish oil, and evidence for their benefit to heart health isn't as strong.
Other supplements may help reduce your blood pressure or cholesterol level, two contributing factors to coronary artery disease. These include:
- Alpha-linolenic acid (ALA)
- Artichoke
- Barley
- Beta-sitosterol (found in oral supplements and some margarines, such as Promise Activ)
- Blond psyllium
- Cocoa
- Coenzyme Q10
- Garlic
- Oat bran (found in oatmeal and whole oats)
- Sitostanol (found in oral supplements and some margarines, such as Benecol)
Preparing for your appointment
Early-stage coronary artery disease often produces no symptoms, so you may not discover you're at risk of the condition until a routine checkup reveals you have high cholesterol or high blood pressure. So it's important to have regular checkups.
If you know you have symptoms of or risk factors for coronary artery disease, you're likely to see your primary care doctor or a general practitioner. Eventually, however, you may be referred toheart specialist (cardiologist).