Hydatidiform Mole
Hydatidiform Mole or Vesicular Mole
It is a pregnancy where chorionic villi are transformed into mass of translucent vesicles like bunch of grapes, the incidence is about 1 in 400.
Etiology-
Unknown. For unknown reasons, the embryo dies in uterus, but the placenta continues to develop. Genetic abnormalities at the time of fertilization may occur.
The following are risk factors-
- Very young or elderly women.
- Disturbed maternal immune mechanisms.
- Cytogenic abnormality.
- Malnutrition and poor socio-economic conditions.
- History of prior Hydatidiform mole.
Pathophysiology
It is a disease of chorion. The cysts begin to form between 3rd to 5th weeks when the foetomaternal circulation normally becomes established. Microscopically villi show proliferation, oedema, degeneration and haemorrhage. Naked eye appearance shows whole uterus filled with multiple chains and clusters of cysts. No trace of embryo, or the amniotic sac. Ovaries show multiple lutein cysts enlargement.
Classification-
Three types-
- Hydatidiform mole
- Invasive mole (Persistent trophoblastic disease)
- Chorio-carcinoma (malignant trophoblastic disease)
Complete Hydatidiform mole-
The cells turn into abnormal tissue in the uterus. The cells normally form the placenta. The tissue is a cluster of fluid-filled cysts that look like grapes. The cluster continues to grow and fill the uterus. The abnormal tissue is not cancer, but may become cancer.
if it is complete it is an ‘EMPTY OVUM’ meaning there is an abnormal sac but no fetus. Studies show that this type often leads to Choriocarcinoma. The HCG levels for this type are also higher than partial.
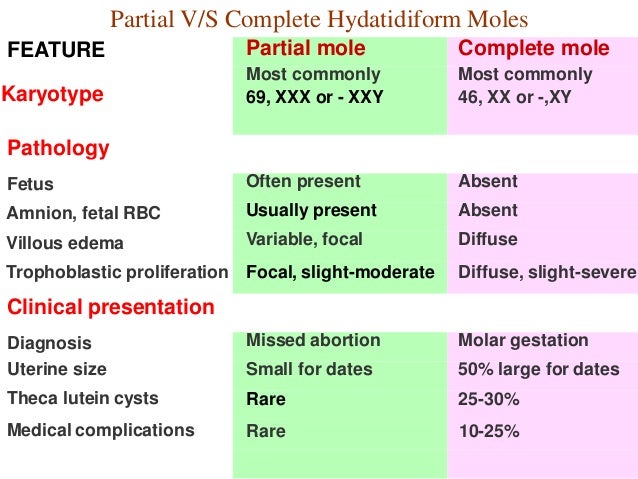
Partial Hydatidiform mole-
In partial mole, normal development of the placental tissue takes place but no fetal tissue development.
If the complete is known to have an empty ovum, partial Hydatidiform Mole has partially formed normal villi with a macerated embryo present. Partially formed because there is a misshapen part of the trophoblast and macerated embryo because the embryo has an abnormally high chromosome level.
Signs and Symptoms
- Pregnancy for 8-12 weeks vaginal bleeding varying from brownish red spotting to heavy bright red. Grape like vesicles may be expelled.
- Varying degree of lower abdominal pain.
- Evidences of anemia, hyperemesis gravidarum and pre-eclampsia may be present.
- Per abdominal examination will reveal the size of uterus is disproportionately enlarged to period of gestation, no foetal parts, no foetal movements felt and no foetal heart sound is audible.
- Vaginal examination shows bloodstained discharge of vesicles.
- Investigations including elevated HCG in urine or serum and sonography are done.
Nursing Interventions
- Assist with client preparations for evacuating the uterus
- Record history, obtain appropriate laboratory tests and participate in physical examinations.
- Nursing diagnosis focuses on knowledge deficit related to consequences of disease, fluid volume deficit, and anxiety.
- Measures to prevent minimize infection be taken.
- Preoperative and postoperative care if hysterectomy is performed.
- Contraceptive counselling.
- Provide information about the disease, necessity for follow-up and the possible consequences.
- Follow-up management for at least two years. The objective is to find out any occurrence of choriocarcinoma. For 4-6 weekly follow up, then monthly follow-up upto a year and lastly after every three months upto 2 years.